SERMs
PRMs
Laparoscopic surgery
Surgery and hormonal treatment
Conclusion
References
Further reading
Endometriosis is an estrogen-dependent disease characterized by the presence of endometrial tissue outside of the uterus that occurs mainly in menstruating women. Both glands and stroma grow in lesions outside of the uterine cavity. These lesions grow and spread as a result of the hormone estrogen. Around 1 in 10 women of reproductive age have endometriosis.
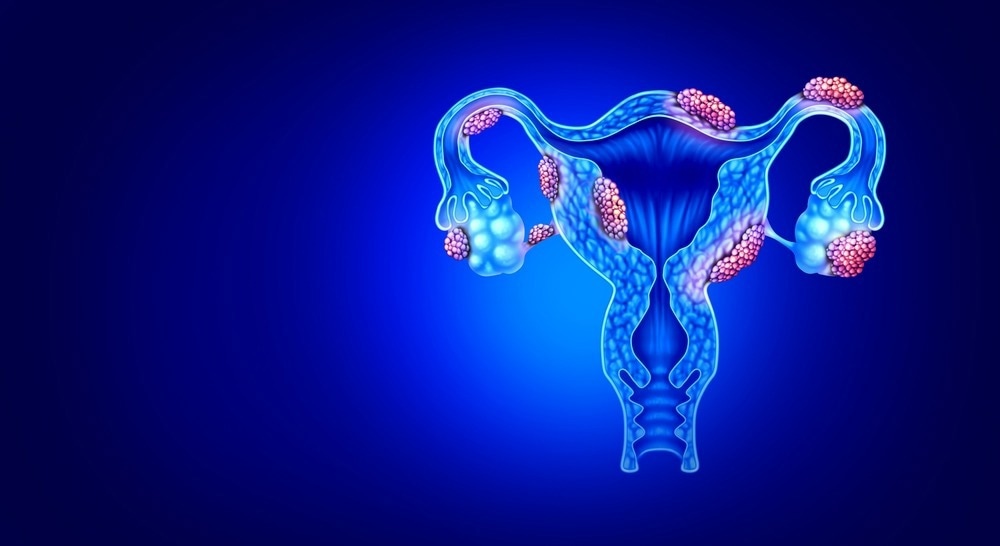
Image Credit: Lightspring/Shutterstock.com
Symptoms are characterized by abdominal and menstrual pain (dysmenorrhoea) and infertility. Non-specific symptoms include lower back pain and pain during or after intercourse (dyspareunia). Medical treatment involves surgical removal of lesions as well as pain relief. Hormonal treatments are utilized to mitigate the effect of estrogen, including oral contraceptive pills, progesterone medication, and intrauterine devices.
SERMs
Selective estrogen receptor modulators (SERMs) can block the effects of estrogen. A review of studies up to May 2020 investigated the evidence behind the therapeutic benefits of SERMs, including only one randomized controlled trial of 93 participants. The study focused on the effect of raloxifene on the symptoms of women post lesion-removal surgery against a placebo.
It was concluded that there was no difference in outcomes for symptoms, recurrence of pain, and overall quality of life indicators. The mental health of the placebo group improved more over 12 months than the raloxifene group. The return of pain post-surgery occurred earlier for women taking the SERM treatment, and the study was prematurely concluded. There was no data to draw conclusions about fertility or focus on effects during pregnancy.
PRMs
Progesterone receptor modulators (PRMs) have antiproliferative effects on the endometrium. These are considered therapeutic agents for endometriosis. A review of studies assessed the efficacy of a range of PRM drugs up to November 2016, and this included ten random controlled trials and 960 participants.
These included mifepristone, asoprisnil ulipristal, leuprolide acetate, gestrinone, danazol, and gonadotropin‐releasing hormone (GnRH) analogs. Asoprisnil and ulipristal studies did not report quality evidence for conclusions. The remaining studies are summarised below.
Mifepristone reduced dysmenorrhoea by roughly 10% and the rate of dyspareunia - although this symptom was highlighted to be recorded as low-quality data. However, the Mifepristone group recorded 24% had hot flushes and 90% experienced amenorrhoea compared to 1% of the placebo group - this was considered high-quality evidence. Further analysis into subgroups suggests that higher doses of 5 or 10mg are more effective in improving dysmenorrhoea or dyspareunia than 2.5mg.
Two studies highlighted low-quality evidence of the efficacies of gestrinone against danazol. Gestrinone had a higher rate of hirsutism and a lower rate of breast reduction. This study showed no significant difference between the drugs for dysmenorrhoea, dyspareunia, pain relief, and secondary symptoms of hot flushes and acne.
Another study of gestrinone against leuprorelin showed gestrinone was more effective on dyspareunia, amenorrhoea, and hot flushes. However, it also caused higher rates of bleeding/spotting and was less effective on dysmenorrhoea than leuprorelin. There was not sufficient evidence to advise on dose-dependent efficacy for gestrinone.
The data for the Mifepristone study was in the moderate quality range. As a result, the author concluded that Mifepristone was the only drug that could be suggested to improve dysmenorrhoea for women with endometriosis. A conclusive result on the optimal dose was not determined.
Laparoscopic surgery
Laparoscopic surgery, or keyhole surgery, is used by surgeons to access abdomen areas without making large incisions. This treatment can physically remove aberrant endometrium growths and reduce associated symptoms.

Image Credit: amab/Shutterstock.com
A review of studies up to April 2020 examined the efficacy of surgical intervention for endometriosis on the symptoms of pain and infertility. This review included results from 14 randomized controlled trials and 1563 women. A common limitation across the studies was the lack of clarity surrounding the method of blinding.
Overall data reports no significant improvement in pain associated with varying levels of endometriosis following surgery. None of the studies investigated the effect on live births. However, there was moderate quality evidence to suggest laparoscopic surgery increased the viability of pregnancies - although results on safety were inconclusive.
Surgery and hormonal treatment
The surgical removal of lesions and hormonal therapy may be administered to patients with endometriosis to alleviate symptoms and manage the condition. The optimal time to deliver hormonal therapy around surgical intervention remains unclear. A review was conducted to determine the most effective timeline for treatment in patients with endometriosis. This review included 25 randomized controlled trials with 3,378 women until November 2019.
Cross-study results showed that hormone therapy delivered after surgery could potentially improve conception rates, pain, and disease recurrence. Data on therapy administered before and around surgery did not produce any statistically significant conclusions. The data quality across the studies ranged from moderate to very weak.
Conclusion
There is no cure for endometriosis, but numerous treatments are available for patients. Studies regarding the safety and efficacy of these treatments, including cross-treatment comparisons, lack of quality means of gathering precise and objective data. However, the conclusions drawn from these studies can help to direct future research.
As this condition is the second most common disease for women of reproductive age, ranging from mild pain to severe symptoms of infertility, dysmenorrhoea, and dyspareunia, there is a pressing need for more conclusive research into highly effective treatments for endometriosis.
References
- Bafort, C., Beebeejaun, Y., Tomassetti, C., Bosteels, J. and Duffy, J., 2020. Laparoscopic surgery for endometriosis. Cochrane Database of Systematic Reviews, 2020(10).
- Chen, I., Veth, V., Choudhry, A., Murji, A., Zakhari, A., Black, A., Agarpao, C. and Maas, J., 2020. Pre- and postsurgical medical therapy for endometriosis surgery. Cochrane Database of Systematic Reviews, 2020(12).
- Fu, J., Song, H., Zhou, M., Zhu, H., Wang, Y., Chen, H. and Huang, W., 2017. Progesterone receptor modulators for endometriosis. Cochrane Database of Systematic Reviews, 2017(7).
- Siedlak, A., Kuc, M., Cyboran, K., Machaj, D. and Płaczek, A., 2022. complementary treatment of endometriosis: diet, physiotherapy and psychological treatment. Journal of Education, Health and Sport, 12(7), pp.989-993.
- van Hoesel, M., Chen, Y., Zheng, A., Wan, Q. and Mourad, S., 2021. Selective oestrogen receptor modulators (SERMs) for endometriosis. Cochrane Database of Systematic Reviews, 2021(5).
Further Reading
Last Updated: Apr 10, 2023