What is Polycystic Ovary Syndrome (PCOS)?
PCOS is a common disorder of the endocrine system in women, affecting between 5% and 15% of reproductive-age women. It is characterized by irregular ovulation (and therefore oligomenorrhea, or irregular menstruation), excess androgen levels, and enlarged follicle-containing ovaries.
Although harmless, the follicles are underdeveloped sacs in which eggs develop and are often unable to release an egg. This lack of ovulation, in turn, leads to lower than usual levels of estrogen and progesterone.
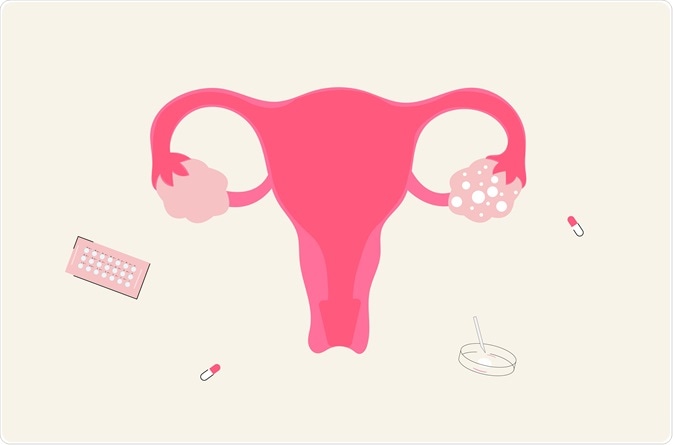
PCOS. Image Credit: Gegambar/Shutterstock.com
Symptoms of PCOS
The onset of symptoms is variable, with some women reporting them in parallel with the onset of menarche, whilst others do not receive a diagnosis until they experience difficulties conceiving. The most common symptoms include:
- Irregular menstruation is defined as a menstrual cycle that continuously falls outside the expected cycle length of 24 – 38 days. This may be accompanied by heavy bleeding when menstruation does occur as the uterine lining grows thicker if not shed regularly.
- Excess hair growth on the face and body is referred to as hirsutism, caused by excess amounts of androgens. Conversely, hair on the scalp may become thinner and fall out.
- Acne typically presenting as inflamed cysts around the jawline, cheeks, and chin. This results from an excess of testosterone which causes overactivity of sebaceous glands.
- Weight gain affects up to 80% of women with PCOS and tends to develop in the abdominal area.
Causes of PCOS
Although the underlying cause of the syndrome remains unknown, several factors that play a role have been identified.
Insulin resistance
The majority of people diagnosed with PCOS present with high insulin levels or insulin resistance, which appears to be both a symptom of PCOS and a physical driver of the syndrome. Under normal hormonal conditions, insulin levels in the blood rise after eating and stimulate muscles and the liver to convert sugar in the blood into energy.
In insulin resistance, the message to stimulate this conversion is faulty, leading to the over-production of insulin by the pancreas. Although an excess of insulin causes weight gain, insulin resistance is observed in both obese and lean women with PCOS, indicating that weight gain is not the sole driver of insulin disruption in PCOS.
Low-grade systemic inflammation
Many studies have demonstrated an elevated biomarker of inflammation in women with PCOS, even once age and body mass index are controlled for. One recent meta-analysis concluded that markers of inflammation are 96% higher in women with PCOS compared to those without the syndrome.
The biomarker, C-reactive protein (CRP) is produced by the liver following stimulation from endocrine cytokines in fat (adipose) tissue, and directly by adipose tissue. Elevated CRP has been observed in women with PCOS in the absence of abnormalities in blood glucose levels or cholesterol, suggesting it could be a marker of early cardiovascular risk.
Indeed, PCOS shares some features with metabolic cardiovascular syndrome (MCS), a cluster of conditions that increase the risk of stroke, type 2 diabetes, and heart disease. Taken together, such findings have raised speculation that inflammation could play a key role in the pathophysiology of PCOS.
Genetics
Family studies have shown a genetic component to PCOS, with the likelihood of developing the syndrome increasing if a first-degree relative is affected. Approximately one-third of women with PCOS have a sister with the syndrome, and approximately one-quarter have a mother with the disorder.
Twin studies have shown that monozygotic twins were twice as likely to both have PCOS than dizygotic twins or sisters. However, as PCOS is a complex and multifactorial syndrome with up to four different phenotypes for diagnosis, a single gene or multiple related genes are unlikely to be identified as causal.
Current thinking suggests that there are hereditary differences in sensitivity to and production of certain hormones including those involved in the brain-ovary connection, those involved in insulin regulation, or variations in how weight and energy are regulated. However, it is likely that all mutations that impact the ovaries, either directly or indirectly, are associated with PCOS.
Epigenetics
Epigenetics refers to how the environment and behavior can alter gene expression. It differs from the permanent changes caused by gene mutations which change the DNA sequence and influence the production of proteins. Instead, epigenetic changes influence how the body responds to a DNA sequence, essentially affecting gene regulation.
Evidence from animal studies suggests that an environmental factor, present during in utero development could lead to changes in gene regulation. Specifically, studies that have exposed female mammals to an excess of androgens in utero have developed clinical phenotypes like those observed in PCOS.
Although the exact mechanism by which this occurs is unknown, researchers hypothesize that excess androgens may impact the Insulin-Like Growth Factor 2 (IGF2) gene which promotes the growth and proliferation of tissue cells. A second hypothesis suggests that androgens alter DNA methylation, a biological process where methyl groups are added to the DNA molecule. This results in a change to DNA activity without altering the DNA sequence.
Polycystic Ovary Syndrome (PCOS) Symptoms
References
- Duleba, A. J., & Dokras, A. (2012). Is PCOS an inflammatory process?. Fertility and sterility, 97(1), 7–12. https://doi.org/10.1016/j.fertnstert.2011.11.023
- González F. (2012). Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids, 77(4), 300–305. https://doi.org/10.1016/j.steroids.2011.12.003
- Kalyan, S., Goshtesabi, A., Sarray, S., Joannou, A., & Almawi, W. Y. (2018). Assessing C reactive protein/albumin ratio as a new biomarker for polycystic ovary syndrome: a case-control study of women from Bahraini medical clinics. BMJ open, 8(10), e021860. https://doi.org/10.1136/bmjopen-2018-021860
- O'Reilly, M. W., Kempegowda, P., Walsh, M., Taylor, A. E., Manolopoulos, K. N., Allwood, J. W., Semple, R. K., Hebenstreit, D., Dunn, W. B., Tomlinson, J. W., & Arlt, W. (2017). AKR1C3-Mediated Adipose Androgen Generation Drives Lipotoxicity in Women With Polycystic Ovary Syndrome. The Journal of clinical endocrinology and metabolism, 102(9), 3327–3339. https://doi.org/10.1210/jc.2017-00947
- Rocha, A. L., Oliveira, F. R., Azevedo, R. C., Silva, V. A., Peres, T. M., Candido, A. L., Gomes, K. B., & Reis, F. M. (2019). Recent advances in the understanding and management of polycystic ovary syndrome. F1000Research, 8, F1000 Faculty Rev-565. https://doi.org/10.12688/f1000research.15318.1
Further Reading
Last Updated: Jan 17, 2022