It was in the 1970s that the angioplasty procedure was started to be used for blocked heart arteries, or coronary arteries, as they are called. It rapidly became a successful procedure in the majority of patients, both because it restored the patency of the blocked blood vessels and because it was much less invasive than conventional open-heart arterial bypass surgery.
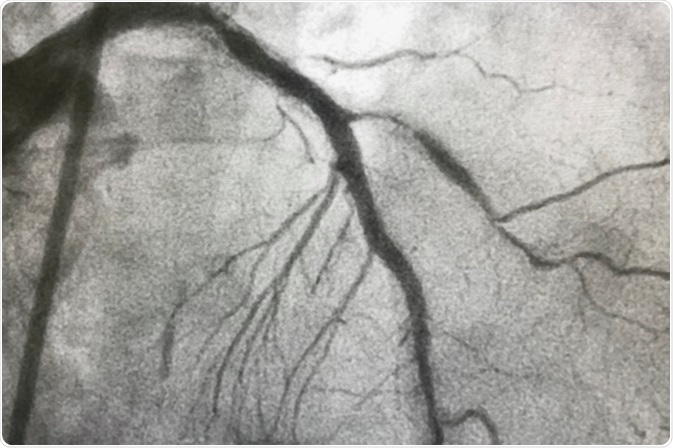
Image Credit: BelezaPoy / Shutterstock
Balloon angioplasty was the first procedure to attain wide application, and consisted of reopening a blocked vessel by inflating a small balloon at the end of a catheter passed into the vessel. However, in several patients, the elastic recoil of the strong elastic fibers in the wall of the artery meant that up to 40% of the widening was lost within a short time.
To counteract this, the arterial stent began to be used. It reduced the rate of recurrent blockage. However, clot formation, or thrombosis, and blockage of the stent still occurred in up to 15% of patients after angioplasty and stenting.
Still later, stents which released drugs (drug-eluting stents) were conceived.
The greatest roadblock so far as far as all these procedures are concerned is the persistent occurrence of restenosis in a percentage of patients. While it is reduced by stenting, it still affects a significant percentage of patients. But what causes it?
Restenosis after balloon angioplasty
The inflation of the balloon inside an artery blocked by an atheromatous plaque literally smashes the atheroma against the arterial wall, and stretches the artery. This causes the atheroma to fracture, with the injury extending deeper into the vessel wall. Thus balloon inflation causes an acute, less controlled and more diffuse type of arterial injury during vessel widening.
Restenosis is caused by elastic recoil of the arterial wall, constriction of the artery due to the formation of fibrous scar tissue (called negative remodeling) and the persistence of the plaque. It is more common after angioplasty than stent placement. Negative remodeling causes a loss of up to 66% of the increase in lumen size. These mechanisms underlie the recurrent blockage or restenosis of the type called post-angioplasty restenosis, or PARS.
Restenosis after stent insertion
In-stent restenosis (ISR) involves an abnormal healing mechanism in response to continuing injury. There are multiple mechanisms which produce and aggravate injury to the vessel wall after stenting:
- injury due to widening and plaque destruction by balloon inflation pressures
- a more focal injury caused by the pressure of the struts of the stent on the vessel wall.
- ongoing injury due to the continuous high distending pressure on the local arterial wall
- the presence of the stent as a foreign body inside the blood vessel, which persists over a long period and produces chronic inflammation
- the presence of a scaffold in the form of a stent, which provides a supporting structure for platelets and connective tissue cells to creep over and extend to form a scar.
Thus a stent produces more lasting and deep injury than the balloon.
Elastic recoil and post-injury vascular constriction are largely prevented by stent placement, so that the lumen remains much wider after this procedure. Thus the mechanism of in-stent restenosis (ISR) is different. Here the contributing players are:
- ongoing inflammation in the vessel wall
- endothelial cell overgrowth over the stent scaffolding
- endothelial cell dysfunction due to prolonged inflammation
- endothelial cell loss exposing bare intima (the innermost layer of the arterial wall, which is normally covered by smooth endothelium) to the flow of blood
- subclinical thrombus (clot) formation
- release of vasoactive and inflammatory factors which signal the smooth muscle cells to transform
- the proliferation of smooth muscle cells in the arterial medial layer
- its migration to the innermost layer (or intima) of the wall to form a neointima
- its transformation from a contractile to a synthetic profile
- abundant extracellular matrix production and collagen fiber synthesis
- formation of a bulging scar which narrows the lumen
Why does healing lead to hyperplastic growth and blockage of the injured artery? The most popular explanation is that it is an exaggeration of a physiological phenomenon that follows injury. While initial endothelial migration to cover the metal surface of the stent is a healthy reaction, and protects against recurrent thrombus formation and blockage, prolonged inflammation causes abnormal hyperplastic neointimal growth and restenosis.
Three phases of inflammation
The early inflammatory phase is marked by platelet aggregation, fibrin deposition and thrombus formation.
The recruitment phase, which occurs over the next 3-10 days, sees additional leukocytes joining the inflammatory response, migration and adhesion of more platelets and leukocytes to the vessel wall. Cellular signals from activated inflammatory cells induce endothelial proliferation. They also produce smooth muscle cell activation, vasoconstriction and coagulation.
The late phase occurs over weeks and months following the injury, and witnesses neointimal hyperplasia. This eventually leads to the formation of bulging scar tissue which blocks the stent or the artery. Oxidative stress is another contributor to endothelial dysfunction and resulting overgrowth of the intima.
There is another major contributor to stent failure, which is late thrombosis. This occurs after drug release from the stent stops, and is precipitated by the loss of endothelium from part of the arterial wall. To counteract this, systemic antiplatelet and anticoagulant agents are continued for a year after stenting with DES.
References
Further Reading
Last Updated: Apr 14, 2021