Retinoic acid has a protective action on the epithelium. Its derivatives are highly effective in treating and preventing ultraviolet-induced damage to the skin following exposure to ultraviolet radiation.
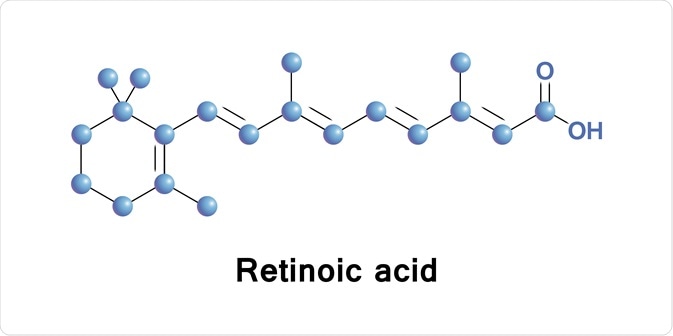 Image Credit: Anastasiya Litvinenka/Shutterstock.com
Image Credit: Anastasiya Litvinenka/Shutterstock.com
Ultraviolet rays act through many mechanisms to damage exposed skin. One chief route is by inducing the AP-1 transcription factor, a protein which stimulates the expression of protein-degrading enzymes called matrix metalloproteinases (MMPs), such as collagenase, gelatinase and stromelysin. These enzymes are crucial to breaking down the collagen fibers and other components of the dermis, which predisposes to skin damage and weakening.
The clinical features which signal ultraviolet damage to skin include:
- The appearance of fine and coarse wrinkles
- Mottling of the skin
- Actinic keratosis
- Freckles
- Roughness
- Telangiectasis or the appearance of fine blood vessels
- Loss of normal skin color
Retinoic acid derivatives are often used topically. They are not well-absorbed through the skin, thus they do not appear to any significant extent in the blood level of retinoic acid or other retinoids. Tretinoin, or all-trans retinoic acid, is a topical retinoid that is extensively used to treat the changes in sunlight-damaged skin. It also inhibits sunlight-induced or ultraviolet-induced damage to skin cells if applied to the skin before exposure.
How does retinoic acid achieve this? Topical retinoids induce keratin-producing cells in the skin to proliferate and to differentiate faster, as well as producing more collagen. Topical tretinoin application produces the greatest visible improvement in the form of less fine wrinkles, improved smoothness of skin and a more even skin color. These are thought to be due to healthy collagen formation. The skin both appears and feels healthier, and firmer. The blood supply to the deep layer of skin is also improved.
Studies have shown that skin really does change on tretinoin therapy. On biopsy, tretinoin at 0.05% and 0.01% both produced an increased thickness in the epidermis. This is because of a higher number of layers in the granular cell layers. At the same time, the melanin content dips, and the stratum corneum, or keratinized superficial layer, becomes firmer. Collagen content is restored to 80% of the original level after tretinoin application to photo-damaged skin.
The new collagen is not disorganized but firmly packed into orderly bundles in the deeper part of the dermis. The collagen changes are due to a reduction in MMP activity by 70-80%, while the opposing enzyme, called tissue inhibitor of MMP type I, or TIMP, remains unchanged.
Retinol is required at a 20-fold higher concentration than retinoic acid derivatives, to achieve comparable results.
 Image Credit: Geinz Angelina/Shutterstock.com
Image Credit: Geinz Angelina/Shutterstock.com
Topical tretinoin is a first-generation anti-acne medication and is used to treat mild to moderate acne with success, and with minimal side effects. It does not increase the levels of retinoic acid in the blood. It relieves acne by producing faster maturation of skin cells, thus increasing the rate of shedding of fully keratinized mature and dead skin cells at the surface, and the expulsion of mature comedones.
13-cis RA, or isotretinoin, is another retinoic acid derivative with unique immunomodulatory and anti-inflammatory actions. Isotretinoin is used orally, and is reserved for more severe acne that is unresponsive to topical therapy. It reduces the number of leukocytes that aggregate at the inflamed site, inhibits the proliferation and differentiation of sebum-producing cells in the sebaceous follicles, and induces death of these cells. Thus it reduces the number of infected and inflamed comedones, shrinks the sebaceous glands and inhibits sebum production. It also stabilizes the keratinization of the epidermal cells.
Its major disadvantage is the oral route of administration, which means it achieves significant blood levels, which can harm developing fetal tissues. In contrast, topical administration achieves at most a blood concentration of 0.015 mg/kg, which is at least 30 times less than the teratogenic dose. In the US, to prevent teratogenicity, isotretinoin users must be registered in a special program to ensure that they are not pregnant. Isotretinoin remains in the body for up to a month after the last dose, requiring precautions to be taken during this period.
Retinoic acid is widely used as an adjunct to treat neuroblastomas, and radio-iodine-resistant thyroid cancers, as well as preventing cancers of the head and neck. It is widely used to prevent the premalignant lesions of actinic keratosis, leukoplakia and cervical dysplasia. Retinoids also delay the appearance of skin cancer when administered to individuals with xeroderma pigmentosum.
Retinoic acid in excess disrupts vital embryonic processes and can produce growth retardation both before and after birth, serious anomalies in many regions of the hindbrain, the back part of the central nervous system, malformed skull and facial skeleton, and heart abnormalities.
Retinoic acid upregulates genes that promote survival in adverse conditions. It induces differentiation, inhibits proliferation, induces apoptosis and has strong antioxidant activity. It also regulates stem cells. They thus have important roles in the prevention and treatment of cancer. They regulate tumor-suppressor genes and thus inhibit tumor growth. Thus they are important in the follow-up chemoprophylaxis of neuroblastomas in children. It induces differentiation of cells, which thus mature and cease to proliferate, and thus is dramatically successful in promyelocytic leukemia treatment.
References
Further Reading
Last Updated: Apr 14, 2021