Rhinitis can be broadly defined as inflammation of the nasal mucosa and is generally categorized as allergic or non-allergic rhinitis. It has been estimated that allergic rhinitis has a high prevalence of between 10 to 40% of the general population, whereas non-allergic rhinitis alone is thought to affect more than 200 million people worldwide.

Image Credit: Emily frost / Shutterstock.com
The prevalence of allergic rhinitis is increasing, and severe cases have been associated with impairments in quality of life, work performance, and sleep patterns of those affected by this condition. Furthermore, non-allergic rhinitis is an underrecognized entity that affects many individuals and is often inadequately treated.
Allergic rhinitis
Allergic rhinitis represents the most common cause of allergic diseases. It is an immunoglobulin E (IgE)-mediated inflammatory chronic illness that affects the nasal mucosa. Allergic rhinitis can be characterized by the presence of rhinorrhea, itching, sneezing, and congestion. A positive correlation between the clinical history and allergen sensitization is usually enough to support the diagnosis of allergic rhinitis.
Upon exposure to an inciting allergen, a plethora of inflammatory cells, such as CD4-positive T cells, B cells, mast cells, macrophages, and eosinophils, infiltrate the nasal lining. Cytokines that are then released promote the production of IgE by plasma cells, triggering the release of inflammatory mediators like histamine and leukotrienes that are responsible for the development of characteristic symptoms.
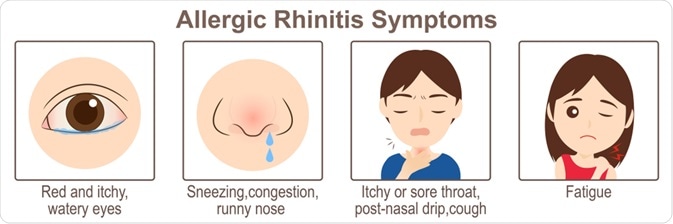
Image Credit: CHEN I CHUN / Shutterstock.com
There are two general types of allergic rhinitis, which include season and perennial allergic rhinitis. Seasonal allergies, which are usually due to cyclic airborne plant pollens, are more common and cause problems to individuals at certain times of the year. Conversely, perennial allergies cause symptoms continuously throughout the year due to constant allergen exposure such as house dust mites, mold spores, cockroaches, cigarette smoke, and pet dander.
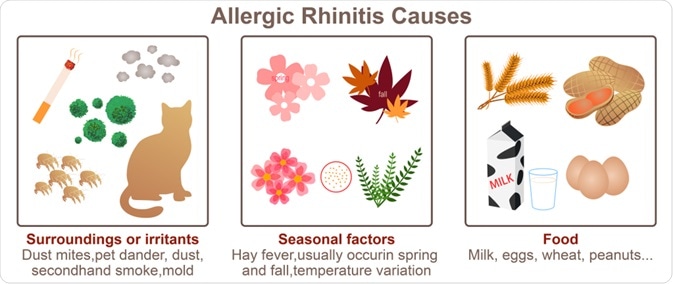
Image Credit: CHEN I CHUN / Shutterstock.com
The Allergic Rhinitis and its Impact on Asthma (ARIA) group classified allergic rhinitis as intermittent and persistent types. Intermitting allergic rhinitis is defined as symptoms lasting less than 4 days per week and for less than 4 weeks. Comparatively, persistent allergic rhinitis will cause symptoms for more than 4 days per week or last for more than 4 weeks, regardless of the number of days per week.
According to the severity of the condition, allergic rhinitis is considered mild when patients generally have a normal sleep pattern and do not encounter trouble while performing their everyday activities in work or school. Such mild symptoms are usually intermittent. On the other hand, moderate or severe allergic rhinitis will significantly affect sleep and the ability of affected individuals to perform their daily activities.
Non-allergic rhinitis
Non-allergic rhinitis syndromes are heterogeneous and often unrelated to each other. The common features of this group of conditions are chronicity and bothersome nasal conditions that do not involve allergic mechanisms. Some research points to neurosensory abnormalities as an important factor in non-allergic rhinopathy; however, they remain a murky group of overlapping syndromes.
Allergy? Maybe not. Could be nonallergic rhinitis
There are at least nine subtypes that fulfill the criteria for non-allergic rhinitis, which include:
- Drug-induced rhinitis
- Gustatory rhinitis (rhinorrhea associated with eating hot and spicy foods)
- Hormonally induced rhinitis, non-allergic rhinitis with eosinophilia syndrome (NARES)
- Senile rhinitis
- Atrophic rhinitis
- Occupational rhinitis
- Infectious rhinitis
- Vasomotor rhinitis
Among these conditions, vasomotor rhinitis, which can also be referred to as idiopathic rhinitis, represents the most commonly diagnosed form of non-allergic rhinitis, accounting for more than half of all the cases. Nasal symptoms of this condition can be sporadic or persistent and are triggered by cold air, sudden changes in temperature, humidity, barometric pressure, alcohol intake, as well as strong emotions.
Rhinitis medicamentosa or drug-induced rhinitis is another common variant of non-allergic rhinitis caused by the rebound nasal congestion that arises due to the chronic overuse of the topical nasal decongestants oxymetazoline or phenylephrine. Moreover, in aspirin-sensitive patients, symptoms of nasal obstruction are quite common.
Non-allergic rhinitis with eosinophilia (NARES) is diagnosed when eosinophils make up between 5 adn 20% of the cells observed on a nasal smear. This condition usually develops in adulthood with year round symptoms such as profuse rhinorrhea and nasal congestion. Serum eosinophil levels can also be elevated in certain instances.
References
Further Reading
Last Updated: May 16, 2021