There are several risk factors that raise the propensity to get skin cancers by manifold. The exact cause of why DNA damage occurs and why cancer results from such DNA damage is not known clearly, but these risk factors give an idea regarding factors that can be avoided to prevent skin cancers.
Risk factors of skin cancers
The risk factors of skin cancers include:-
Exposure to sunlight
One of the significant risk factors for skin cancer is exposure to sunlight (UV radiation). This is particularly true for basal cell and squamous cell cancers that occur in exposed parts of the skin.
Sunlight is a source of UV radiation. This UV radiation exposure leads to damage to the DNA of the skin cells. DNA damage is the underlying cause of any cancer.
Sunlight exposure may be direct or may be indirect. Indirect exposure results from reflected sunrays by sand, water, snow, ice, and shiny surfaces like glass. The sun exposure is also high at higher elevations, such as in the mountains. The sun's rays can penetrate through clouds, windshields, windows, and even light clothing. Australia had the highest overall rate of non-melanoma skin cancer in 2020, followed by New Zealand.
Those with a propensity for severe sunburns and blisters on exposure to sunlight are at a heightened risk of skin cancers. People who burn easily are more likely to have had sunburn as a child. The total amount of sun exposure over a lifetime is a risk factor for skin cancer. Those overexposed to the sun during childhood are at greater risk. It is found that most of the sun's UV radiation exposure occurs before the age of 18 years.
Studies have shown that a tan slightly lowers the risk of sunburn, but the risk remains. People who tan little or not at all and burn more when exposed to the sun are more at risk of skin cancers.
Exposure to Sunlamps and tanning booths
These artificial sources of UV radiation can cause sun damage to the skin and may raise the risk of skin cancers. Healthcare providers strongly encourage young individuals, especially, to avoid using sunlamps and tanning booths. The risk is high in users of sunlamps and tanning booths before the age of 30. Early exposure to these artificial UV sources can significantly accelerate the skin aging process and increase the accumulation of DNA damage over time, further amplifying the risk of developing skin cancer at a younger age compared to those with minimal to no such exposure.
 Image Credit: Lucky Business / Shutterstock
Image Credit: Lucky Business / Shutterstock
Family history of skin cancer
Those with a family history of skin cancers are at a raised risk of skin cancers. Melanoma sometimes runs in families. Having two or more close relatives or first-degree relatives (parents, siblings, or offspring) raises the risk of melanoma. Other types of skin cancer also sometimes run in families. Those with a family history of xeroderma pigmentosum or nevoid basal cell carcinoma syndrome have skin that is more sensitive to the sun, which increases the risk of skin cancer.
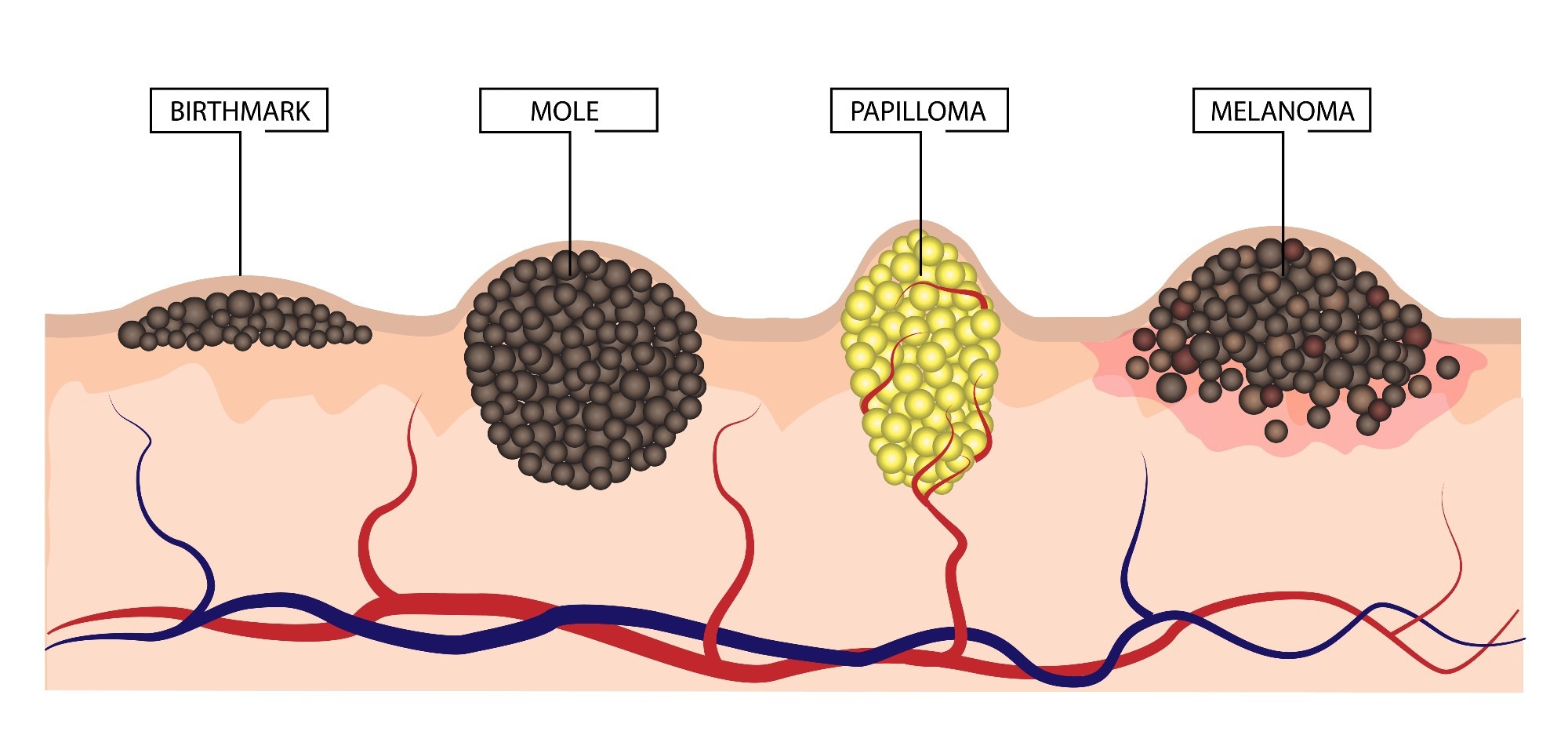 Diagram of birthmark, mole, papilloma and melanoma. Image Credit: LiliiaKyrylenko / Shutterstock
Diagram of birthmark, mole, papilloma and melanoma. Image Credit: LiliiaKyrylenko / Shutterstock
Previous melanoma
Individuals who have had melanoma before are at a greater risk of getting it again. This elevated risk persists because the initial melanoma may indicate an inherent susceptibility to skin cancer, either due to genetic factors, a compromised immune system, or lifestyle factors that continue to expose the skin to harmful UV radiation.
Age and sex
Men are more susceptible to both melanoma and non-melanoma skin cancers. Melanomas can be found in younger people, but the rates of all types of skin cancer rise with increasing age. This increased susceptibility in men may be attributed to higher cumulative sun exposure and less likelihood of using sun protection, coupled with a tendency to ignore or delay seeking medical advice for suspicious skin lesions.
Skin colour
Individuals with fair or pale skin, especially with blonde, red, or light-brown hair and blue, green, or gray eyes, are at a raised risk. Additionally, this demographic tends to accumulate sun damage more quickly than those with darker complexions, significantly increasing their likelihood of developing both melanoma and non-melanoma skin cancers over time.
Certain medications
Some diseases and medications, such as antibiotics, hormones, or antidepressants, may make the skin more sensitive to sun exposure and raise the risk of skin cancers. This increased sensitivity, known as photosensitivity, can lead to more severe and rapid sunburns under exposure to UV radiation, acting as a catalyst for the DNA damage that precipitates skin cancer development.
Dysplastic nevus
Individuals with a dysplastic nevus are at a raised risk of getting melanoma. This type of mole looks different from an ordinary mole. It is more prominent, and its edges, structure, surface, etc., may differ. It may be longer and wider with patches of several colors ranging from shades of pink to dark brown. The surface is smooth, scrappy, or pebbly, and the edges are rough and blurred. A dysplastic nevus is more likely than a common mole to become cancerous.
Over 50 moles on the body
Individuals with more than 50 moles on their body are more at risk of melanomas. This is because having a higher number of moles increases the likelihood of one or more evolving into malignant melanoma, especially if any of the moles exhibit atypical features such as irregular shape, color, or size.
Old large scars
The presence of old large scars, ulcers, burn marks, and skin inflammations raises the risk of squamous and basal cell cancers. Scarred or previously damaged skin areas have compromised protective barriers and cellular changes, making them more susceptible to the carcinogenic effects of UV radiation and, thus, more prone to developing these types of skin cancer.
Arsenic exposure
Arsenic exposure raises the risk of basal cell or squamous cell cancers. Long-term exposure to high levels of arsenic, commonly found in contaminated well water and industrial pollutants, can lead to skin changes and lesions that predispose individuals to these types of skin cancer, even years after the exposure has ceased.
Radiation exposure
Radiation exposure to the skin for other cancers may damage the skin to cause cancers. This damage often results from therapeutic radiation treatments for other types of cancer, where the ionizing radiation can lead to DNA mutations in skin cells, significantly increasing the risk of developing secondary skin cancers in the treated areas.
Actinic keratosis
Those with Actinic keratosis (a flat, scaly growth on the skin in the exposed areas such as the face and the backs of the hands) are at a raised risk of squamous cell cancer. Actinic keratosis is considered a precancerous condition; if left untreated, it has the potential to progress to squamous cell carcinoma, emphasizing the importance of early detection and treatment to prevent the development of skin cancer.
Human papillomavirus (HPV)
Exposure to human papillomavirus or HPV also raises the risk of squamous cell skin cancer. These HPVs are different from the HPV types that cause cervical cancer in the female reproductive tract. Specifically, HPVs that infect the skin can cause warts and lesions that, over time, may undergo malignant transformation into squamous cell carcinoma, especially in individuals with weakened immune systems.
What Does Skin Cancer Look Like?
Sources
- Skin Cancer (Including Melanoma)—Patient Version.” National Cancer Institute, Cancer.gov, 2019, https://www.cancer.gov/
- Sunsmart. “Prevent Skin Cancer & Sunburn This Summer - SunSmart.” Prevent Skin Cancer & Sunburn This Summer - SunSmart, 2019, https://www.sunsmart.com.au/
- World Cancer Research Fund International. “Skin Cancer Statistics | World Cancer Research Fund International.” WCRF International, 2020, - https://www.wcrf.org/cancer-trends/skin-cancer-statistics/
Further Reading
Last Updated: Feb 28, 2024