Small fiber neuropathy (SFN) is a form of neuropathy which primarily affects the small nerve fibers of the peripheral nervous system. Small nerve fibers are responsible for carrying pain and temperature sensations.
Small nerve fibers are also responsible for regulating the functioning of sweat glands, heart, gastrointestinal organs, and blood vessels.
Small fiber neuropathy occurs due to the selective destruction of small myelinated A-delta or unmyelinated C fibers.Usually small nerve fiber results in the destruction of small nerve fibers; only rarely is the destruction of large nerve fibers observed.
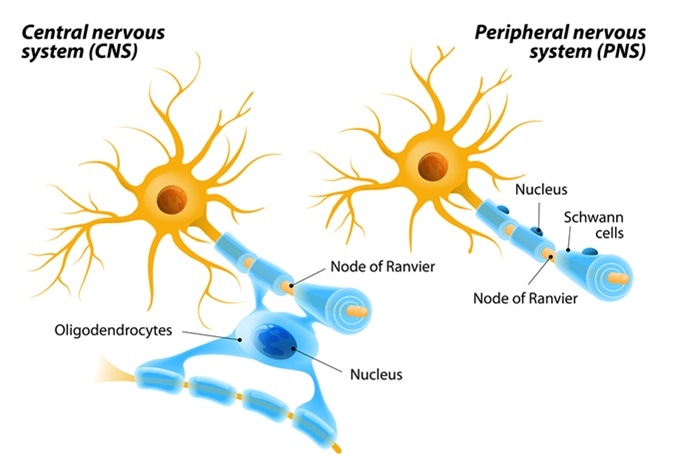
Oligodendrocytes in the central nervous system and Schwann cells in the peripheral nervous system.. Image Credit: Designua / Shutterstock
Diagnosis of SFN
Physicians usually take a complete medical history and do a thorough physical examination before confirming SFN. Evaluation of the complete medical history is of paramount importance in diagnosing SFN as it may reveal underlying conditions causing SFN such as diabetes, HIV, metabolic syndrome, hepatitis C virus infection, or a past record of neurotoxic drug exposure.
Following clinical examination, ancillary testing is useful to confirm the diagnosis in complex cases.
Quantitative Sensory Testing
Quantitative sensory testing (QST) is a psychophysical assessment test done to detect the functioning of somatosensory nervous system. QST can reveal the threshold levels of thermal sensation, thermal pain and vibratory sensation. A wide range of mechanical and thermal tests, non-nociceptive and nociceptive of calculated intensity provides an evaluation of Aβ-fibres, Aδ-fibres and C-fibres and their analogous central pathways.
Electromyography and Nerve Conduction Studies
As SFN usually involves small nerve fibers, routine nerve conduction studies and electromyography is performed to detect the functioning of large nerve fibers. These tests are primarily conducted to detect large nerve fiber involvement. Only when the involvement of large nerves is ruled out, can appropriate disease evaluation, treatment planning, and prognosis be achieved.
Two further tests which can accurately detect small nerve fiber involvement to confirm SFN are skin biopsy testing, which can detect the intraepidermal nerve fiber density, and quantitative sudomotor axon reflex testing (QSART), which is performed to evaluate sudomotor autonomic function.
Skin Biopsy Testing
This test is invasive: usually, punch biopsies of 3 mm diameter are removed from the distal part of the leg, thigh, and proximal thigh of one lower limb. The biopsy specimens are subjected to immunostaining using an antibody against protein gene product 9.5 (a panaxonal marker). Further, the number of small nerve fibers is calculated with high-definition microscopes. Also, intraepithelial nerve fiber densities are measured and calculated with normal values.
SFN is suspected when intraepithelial nerve fiber densities fall below the expected range. Even though SFN nerve fiber density sometimes shows normal values in the initial stages, the biopsy test may reveal some atypical morphological changes that could indicate SFN. It is recommended that a repeat biopsy be performed after 6 to 12 months to confirm the diagnosis in such cases.
Skin biopsy testing has 88 percent accuracy over quantitative sensory testing in detecting SFN.
Quantitative Sudomotor Axon Reflex Testing (QSART)
This test measures postganglionic sympathetic cholinergic functioning. A mild electric current is passed through the skin to extract acetylcholine (a charged substance). Iontophoresis induced by acetylcholine results in local sweating because of the stimulation of local sweat glands.
This stimulation also activates the axon reflex which results in sweat production in the nearby sweat glands. Further, the sweat output is assessed by the passage of dry gas over the regions which have not been stimulated, and the change in humidity is measured during the process. One study showed that QSART was atypical in 74% of patients with SFN.
Basic Investigations to Confirm SFN
Once an accurate diagnosis is achieved, further evaluation should be done to find out the exact cause of disease. Basic tests typically consist of:
- Complete blood cell count
- Metabolic disease assessment
- Lipid profile
- Erythrocyte sedimentation rate
- Thyroid-stimulating hormone level
- Free thyroxine (T4) level
- Antinuclear antibody
- Extractable nuclear antigens
- Angiotensin-converting enzyme (ACE) level
- Serum and urine immunofixation examination
- Level of Vitamin B12
- 2-hour oral glucose tolerance test.
Some specialized tests should also be considered to accurately identify the cause of SFN. In case of gastrointestinal disturbances, an evaluation of gliadin antibody and tissue transglutaminase antibodies should be performed along with a small-bowel biopsy. Also, serological testing should be conducted in high-risk HIV and Hepatitis C patients. Genetic testing in case of a positive family history, and lip or bone marrow biopsy in case of Sjogren disease, seronegative sicca syndrome, or amyloidosis, must be performed.
Treatment of SFN
Treatment of SFN should be aimed at treating the fundamental cause, and pain management. Treating the cause ensures that disease progression is slowed down. Some measures which should be considered while treating SFN include:
- Controlling diabetes, prediabetes and metabolic syndrome-A deranged glucose metabolism is one of the leading cause of SFN, hence life style alterations, appropriate medications, and weight control measures should be taken to control the spiking glucose levels. It has been observed that diabetic neuropathy can be reversed by the introduction of appropriate life-style modifications. Regular exercise and weight control have also been found to control metabolic syndrome related SFN.
- Treating other conditions-A treatment plan aimed at treating other conditions that cause or accompany SFN, such as sarcoidosis, autoimmune diseases, and celiac disease, have also resulted in an overall improvement of the symptoms of SFN.
- Management of Pain- Pain control is one of the most important aspects in treating SFN. Pain control is done with the help of a multidisciplinary team which usually involves a physician, neurologist, physiotherapist and psychiatrist. A wide range of medications may be used, coupled with physiotherapy, such as transcutaneous electrical nerve stimulation (TENS) and hot and cold applications, to manage pain. Antidepressants, anticonvulsants, topical anesthetics, narcotic and non-narcotic analgesics, and antiarrhythmics are some of the drugs used in treating SFN.
Further Reading
Last Updated: Dec 9, 2022