In general, the diagnosis of lung cancer, particularly when multiple pulmonary sites are involved, can be challenging to define. The staging of lung cancer is therefore crucial in not only providing an accurate diagnosis and prognosis for patients but is also used to determine the best treatment protocol.
.jpg)
Image Credit: create jobs 51/Shutterstock.com
Importance of staging
Staging of cancer is a crucial component of the diagnostic process that provides a standardized approach to define the anatomic extent of the disease. Additionally, cancer staging allows healthcare providers to determine the best treatment for his/her patient and, during clinical trials, correlate similar outcomes with patients of a certain cancer stage.
Although recent advancements in molecular biology and the immunologic variability between cancers have enhanced the current understanding of lung cancer, staging remains a fundamental point of care for all cancer patients.
When does staging occur?
The context of when the lung cancer staging occurs is crucial to interpreting the extent of the disease and determining the patient’s course of treatment. The five different types of situations that will be denoted as a prefix to a patient’s cancer stage description include those determined during the clinical (c) or pathologic stage (p), after a patient has received treatment (y), after recurrence (r) and at autopsy (a).
During the clinical stage, for example, factors including any medical comorbidities, tumor-level factors such as specific molecular mutations that can be used as treatment targets, and imaging results can be used to determine the best treatment options for a newly diagnosed patient.
Comparatively, the pathologic stage can only be conducted in patients who have undergone surgical resection of the primary tumor. Patients who undergo tumor resection procedures will typically have both the clinical and pathologic staging performed, with the latter option being more accurate in identifying the extent of tumor growth.
The TMN system
The three components that are incorporated into the lung cancer staging process include tumor (T), node (N), and metastasis (M).
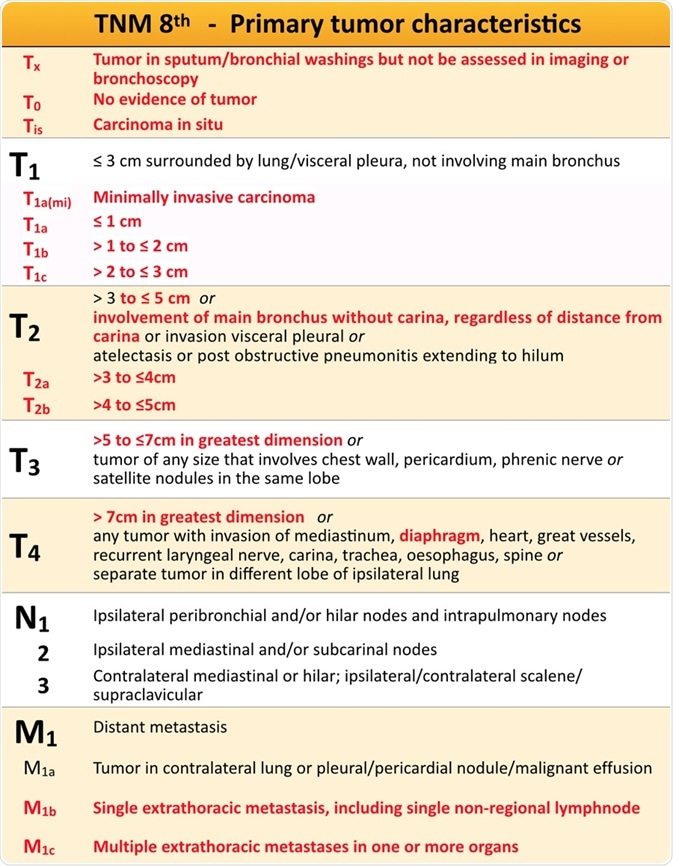
Image Credit: https://radiologyassistant.nl/chest/lung-cancer/tnm-classification-8th-edition
T component
The T component of lung cancer staging describes the extent of the primary tumor and includes 5 categories of T0 to T4. The factors that determine the T component include the size of the primary tumor, whether any satellite lesions are present within the lung parenchyma, as well as whether the primary tumor has extended into nearby thoracic structures.
In terms of primary tumor size, T1 represents tumors that are less than are equal to 3 centimeters (cm) in diameter, whereas T2 designates tumors that are within the range of 3 to 5 cm. T3 primary tumors will be within the range of 5 and 7 cm, whereas the T4 designation is used to represent a primary tumor exceeding 7 cm in size.
In addition to the primary tumor, satellite lesions, particularly pulmonary nodules that are present in the ipsilateral lung, also play a key role in determining the T component of a patient’s lung cancer staging. It is not uncommon to find small pulmonary nodules, especially in patients with a history of smoking.
Cancer cells that have invaded the airway distal to the carina will be assigned a T component of T2A, whereas direct involvement of the tumor burden within the carina or the trachea will receive a designation of T4. In the event that a primary tumor that is less than 5 cm in size is confined to the visceral pleura, a T component of T2 will typically be assigned.
Comparatively, tumors exceeding 5 cm in size that extend beyond the visceral pleura can be staged as either T3 or T4.
N component
The N component represents the extent that cancer has been identified in the thorax and/or supraclavicular lymph nodes. In the absence of metastatic disease, the identification of cancerous nodes is key in stage assessment, and subsequent treatment decisions.
The N component can be further classified into five descriptors, of which include N0, N1, N2, N3, or NX. N0 is used to describe lung cancer that has no apparent lymph node involvement, Comparatively, N1 describes lung cancer that has also been identified in the ipsilateral intrapulmonary or hilar nodes.
An N2 designation represents cancer involvement within the ipsilateral mediastinal or subcarinal nodes. Finally, N3 describes cancer involvement in the contralateral hilar/mediastinal nodes or the supraclavicular nodes. A patient who has been assigned an NX component did not have nodal involvement of their cancer assessed.
M component
The M component describes the state of lung cancer metastasis. Whereas TX and NX designations can be used when there is a lack of clinical staging information, MX is not a recommended designation, as patient history and physical examination should always be available. Typically, metastatic disease is suspected when the patient presents with systemic symptoms like weight loss, loss of appetite, severe fatigue, or other organ-specific complaints.
Like the T and N components, the M component can also be further subdivided into four descriptors, which include M0, M1a, M1b, and M1c. The designation M0 represents a patient with no identifiable distant metastases. In the event that a patient presents with malignant effusion or nodules within the pleural/pericardial regions or separate tumor nodules in a contralateral lobe, the designation of M1a is used.
Comparatively, M1b is used to describe a patient with oligometastasis, which indicates the presence of a single metastatic lesion outside of the thoracic cavity. Finally, the designation M1c indicates that a patient has multiple metastases present in 1 or more organs outside of the thoracic cavity.
R component
Outside of the TMN system can also include the R designation, which is used to identify patients who have undergone some level of surgical resection. The designation R0, for example, identifies a patient who has undergone complete resection of the tumor and has negative surgical margins, meaning that no microscopic or gross evidence of residual tumor has been identified.
Comparatively, R1 represents a patient who has undergone tumor resection but still has residual microscopic disease present, typically surrounding the surgical margins.
The final R designation is R2, which can be identified after a patient has undergone tumor resection but there remains visible and/or palpable tumor. It should be noted that in lung cancer patients, a surgeon will typically avoid surgical resection procedures unless it is anticipated to be curative.
Therefore, an R2 resection will typically occur when the surgeon encounters certain anatomic factors during the operation that prevent him/her from completing the total resection of the tumor.
References and Further Reading
Further Reading
Last Updated: Aug 17, 2020