Skip to:
Breast cancer is among the leading causes of death among women between 25 and 65 years, with an expected incidence of 1 in 8 women in most countries. Screening and early diagnosis are still the best way to reduce the number of breast cancer deaths. However, there is some debate over the best method of screening patients for this disease.
Mammography is currently the most widely accepted screening technique. The US Food and Drug Administration, along with many other national societies, still describes it as the most effective screening test for breast cancer. Yet some doctors have advocated using Thermography despite a lack of evidence that it can reliably detect breast cancer as sensitively as mammography.
What is Mammography?
Mammography is a radiographic method which uses low-dose X-rays to image the breast tissue for both screening and diagnosis of breast cancer. Any suspicious high density regions or unusual patterns such as microcalcifications are examined carefully. These could be due to a range of abnormalities, such as tumors (benign and malignant), fibroadenomas, or cysts with solid areas.
A good mammogram requires firm breast compression against the detector. This minimizes breast movement and allows for the clearest image, it also provides the shortest distance between the breast and detector at all points, reducing the number of films and radiation exposure, while allowing single-plane imaging of the whole breast.
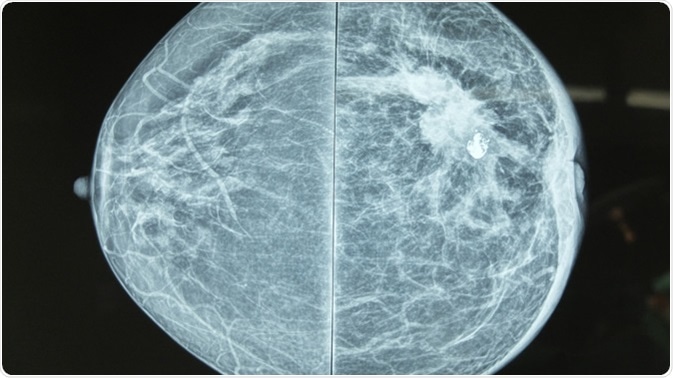
Mammography image showing left breast calcification to suggest malignancy. Image Credit: Casa Nayafana / Shutterstock
Variants of Mammography
Digital mammography uses solid-state detectors rather than an X-ray plate, converting X-rays to electronic signals that are further converted by a computer into digitally displayed and stored images. This technique has several advantages: better contrast for image clarity, easy sharing of images for better diagnosis, long-term image storage, and no film-related issues like overexposure or poor development. This limits the number of mammograms taken which lowers overall radiation exposure, and may be superior for young women and for those with dense breasts.
3D mammography or digital breast tomosynthesis is another technique that employs angled X-rays angled to provide images in the form of a series of thin slices like the well-known CT scan. However, unlike CT, X-ray exposure is very low, especially to the rest of the breast, as with conventional mammography. This technique is still being evaluated for any benefit in terms of diagnostic accuracy and detection rate.
Mammography pros and cons
Mammography equipment is high-maintenance and costly. Sensitivity is reduced in when scanning dense breasts, or in young women. False positives occur in about 10% of cases, causing unnecessary testing, increased costs, and significant emotional and physical distress.
Mammography may also result in overtreating small tumors which could otherwise have been safely ignored, since there is no way to differentiate these from those tumors that require treatment. False-negatives (missing a tumour) occur in about 20% of screening mammograms, especially in very dense breasts and in younger women.
Mammograms also cause radiation exposure, which is most dangerous among women under 40 years. In this group a diagnostic mammogram is valuable if it helps rule out cancer in a breast lump or picks up an early small cancer, but not a screening mammogram. Above this age, the risk of missing a breast cancer is higher than the small risk of mammography, which is proved to have saved up to a third of lives by early detection.
What is Thermography?
Thermography is an imaging procedure first described in 1957 that screens for cancerous tissue using temperature differences at the breast surface, detected by infrared cameras. Malignancies are usually warmer than normal tissue due to the production of NO (nitrous oxide) which produces local vasodilation first, and then promotes blood vessel growth, leading to increased blood flow through the tumor, as well as the higher rate of metabolism in cancer cells. Better equipment and image processing methods have improved the performance of thermography, such as with digital infrared thermal imaging (DITI). However, thermography has not been approved anywhere as a primary screening tool for breast cancer.
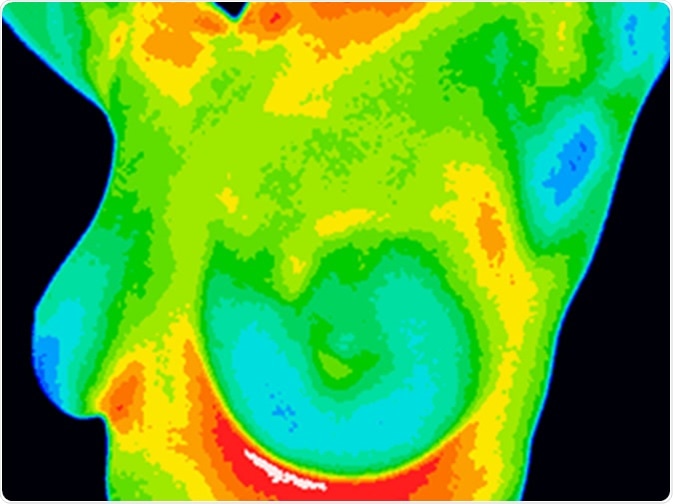
Thermographic image of a chest showing different temperatures from blue showing cold to red showing hot which can indicate inflammation and infection. Image showing healthy breast with no growths. Image Credit: Anita van den Broek / Shutterstock
Thermography: pros and cons
Thermography, especially DITI, is non-invasive, does not involve radiation exposure, is inexpensive, and more accessible to patients.
However, heat recordings may change with inflammation, infection, exercise, or sometimes hormonal changes. Thermography is not adequate for certain situations like older or morbidly obese women, those with larger cancers, breast implants and large or pendulous breasts. It cannot pick up very small cancers or those buried in the breast tissue.
Its sensitivity and specificity are still not comparable to those of mammography. On the other hand, it is capable of picking up asymmetric increases in heat in the breasts, which could alert women to the need for serial screening years before a cancer is detectable by mammography.
Why is Thermography not the Preferred Method of Breast Cancer Screening?
Thermography, or digital infrared thermal imaging, was initially thought to be a good alternative to mammography. In fact, many studies reported it to be as sensitive as 97%, especially with respect to younger women. However, this has not been borne out by large meta-analyses, as well as by later studies.
At present, the detection rate for thermography is only 42% to 80% of cancers, as against 82% to 93% with mammography. Its false positive rate is 25%, more than double that of mammography. No evidence exists that it can reliably detect breast cancer as sensitively as mammography.
According to Helen Barr, head of the quality standards division for mammography in the FDA, “Plenty of evidence shows that mammography is still the most effective screening method for detecting breast cancer in its early, most treatable stages. You should not rely solely on thermography for the screening or diagnosis of breast cancer.”
In fact, the FDA cites thermography as an adjunctive or additional tool which should not be used alone to rule out breast cancer.
Mammograms vs Thermography (Guest: Gaye Walden) | THE HEALTH AWAKENING | Ep. 110
Further Reading
Last Updated: Aug 26, 2019