Bladder cancer is initiated when the cells of the bladder lining begin to grow uncontrollably, forming a tumor. This tumor then continues to grow, entering the muscle and the bloodstream, eventually metastasizing to other organs in the body.
In addition to the risks associated with the cancer itself, it has also been shown that bladder cancer dramatically increases the risk of thromboembolism, which can be life-threatening. As well as tackling the risk of the cancer itself, the other associated conditions must be successfully managed to improve patient prognosis.
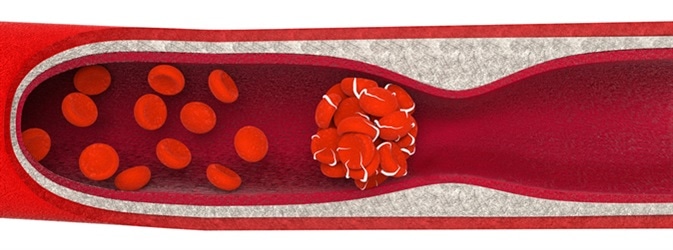
Thromboembolism, a blood clot. Image Credit: Anton Nalivayko / Shutterstock
What is a thromboembolism?
The formation of a blood clot is called thrombosis, which usually occurs in response to blood vessel damage to prevent blood loss. Platelets and fibrin form a clot that clogs up the hole in the vessel wall, preventing the blood from leaking out into surrounding tissues. This clotting system is usually highly controlled, however, occasionally a clot can form without blood vessel damage, or a correctly formed clot can break off the vessel lining.
As the clot travels around the blood system, it can become lodged in the wall of a vessel and block the flow of blood, which is called an embolism. Combining the terms “thrombosis” and “embolism” gives the term “thromboembolism”, which is described as a blood clot blocking a blood vessel and preventing blood flow. This can occur in both veins and arteries, leading to many serious consequences due to a lack of oxygen and waste transport.
Bladder cancer increases risk of thromboembolisms
There are many different risk factors involved in the occurrence of thromboembolism; however, one major risk factor is bladder cancer. 8/100 patients with bladder cancer have a venous thromboembolism, most frequently within the first 6 months of bladder cancer diagnosis. There are many different reasons for this increased risk, including metastasis increasing the coagulability of blood cells, and treatment options such as pelvic surgery (cystectomy) and cisplatin chemotherapy.
Coagulability is vastly increased in cancerous cells, due to many factors. Firstly, tumor cells themselves produce several clotting factors, which stimulate coagulation and clot formation. They also increase inflammation and produce cytokines, affect the blood flow making it more stagnant, and stimulate clot formation. All of these factors mean that the formation of a blood clot is more likely, leading to an increased risk of an embolism.
Cystectomy is a common procedure in patients with bladder cancer, in which all or part of the bladder is removed. This is frequently carried out for biopsies, for example, which are the gold standard for bladder cancer diagnosis. This surgery is associated with increased blood clots for several reasons. For example, this surgery leads to inactivity, which decreases the flow of blood and increases the risk of blood clots.
Additionally, chemotherapy treatments, such as cisplatin, can also increase the risk of blood clot formation. Cisplatin was first licensed for cancer treatment in 1978 and has since grown in popularity to treat many different cancer types, including ovarian, lung, gastric, testicular, esophageal, and bladder cancer.
However, this treatment is known to lead to a dramatic increase in the formation of blood clots, resulting in an increase in thromboembolism risk. One study by Michigan State University showed that there was an 18.8% increased thrombosis rate in 932 patients who received cisplatin. This increase is due to the thrombogenic effect of this drug, leading to vessel lining damage and platelet activation.
Treatment for thromboembolism in cancer patients
The risk of blood clot formation can be reduced through numerous therapies, such as heparin and warfarin, which both function to prevent blood coagulation and break down existing clots. Additionally, compression stockings and mechanical foot pumps can also help lower deep vein thrombosis risk.
Thromboembolic Complications in Bladder Cancer
Further Reading
Last Updated: Dec 13, 2022