An autoimmune disease occurs when the immune system mistakenly attacks and kills the body’s own cells. With the advance in translational research, it is now possible to treat people with autoimmune disorders via targeted and personalized medicines.
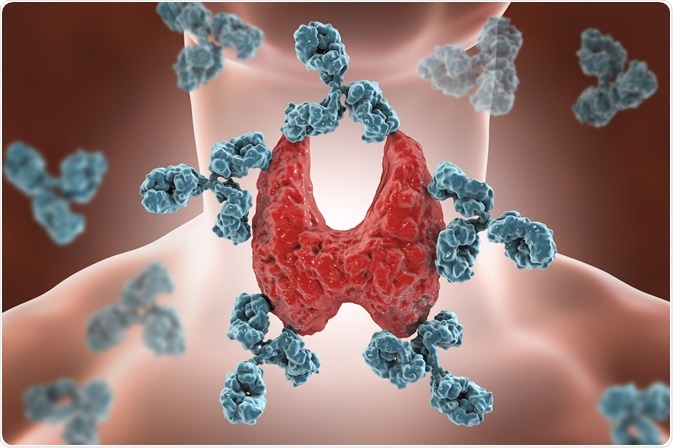
Image Credit: Kateryna Kon/Shutterstock.com
What is an autoimmune disease?
The immune system is designed to protect the body from harmful substances, such as bacteria, viruses, fungi, parasites, environmental toxins, cancer cells, etc. An autoimmune disorder occurs when the immune system fails to differentiate between self and non-self-substances, leading to the destruction of its body cells.
Although the exact etiology of autoimmune disorder is unknown, certain factors can increase the risk of developing the condition. For example, some people are genetically predisposed to develop autoimmune disorders.
However, environmental factors work in synergy with genetic factors to increase the risk. Moreover, it is generally believed that the onset of autoimmune disorders can be triggered by pathogen- or drug-induced changes in normal immune functioning.
What are the treatment options for autoimmune disorders?
Although there is no permanent cure for autoimmune disorders, standard treatments aim at reducing the signs and symptoms of the disease and restrict the autoimmune processes.
To reduce the intensity of damage caused by abnormal immune system functioning, doctors often prescribe immunosuppressive medicines, such as corticosteroids. Pain-relieving medicines are also effective in reducing bone, joint, or muscular pain. Autoimmune disorders associated with inflammation (rheumatoid arthritis) can be treated with medicines that target proteins responsible for joint inflammation, such as TNF blockers.
If autoimmune disorder causes a reduction in important cellular components, such as thyroid hormone, insulin, or vitamin B12, doctors may prescribe supplements to replenish them. In the case of mobility-related problems, physical therapies can be useful.
However, immunosuppressive medicines, which are presently considered as the golden standard for treating autoimmune disorder patients, are mostly associated with harmful side-effects, and long-term use of these medicines can potentially increase the risk of developing deadly infections and cancers.
To overcome the shortcoming of current treatment strategies, new therapeutic interventions are emerging, which function mainly by inhibiting pathogenic cells involved in autoimmune reactions.
Costimulatory blockade
One such approach is treating T cell-mediated autoimmunity. In T cell-based immunity, T cells are activated primarily by two types of signaling pathways: a primary antigen recognition signaling through T cell receptor and secondary costimulatory signaling through antigen-presenting cells.
In the absence of a costimulatory signal, T cells are insufficiently activated, leading to anergy. Two coreceptors of the immunoglobulin family (CD28 and CTLA-4) and their ligands (CD80 and CD86) play a crucial role in mediating the costimulatory activation of T cells. Development of a chimeric fusion protein, CTLA-4-IgG1, for treating people with autoimmune disorders is one of the biggest achievements in the medical field.
This fusion protein binds to CD80 and CD86 with high affinity and prevents them from binding CD28, leading to inhibition of autoreactive T cell activation.
Regulatory T cell augmentation
Another important approach is to increase the number of regulatory T cells. In this regulatory T cell therapy, polyclonal regulatory T cells are isolated from blood samples using specific cell surface markers. Isolated T cells are then expanded experimentally and administered to patients suffering from autoimmune disorders.
The main aim of this method is to increase the ratio of regulatory T cells to pathogenic/effector T cells so that the overall homeostasis of the immune system can be restored.
Antigen-induced tolerance
The main aim of this approach is to identify self-antigens that are targeted in autoimmune diseases, as well as to administer these self-antigens to patients to inhibit autoimmune responses.
Studies have found that repeated exposure to self-antigens can increase the number of antigen-specific regulatory T cells, which in turn can inhibit the ongoing autoimmune responses. These self-antigens can also be modified to induce self-tolerance more effectively.
Manipulation of interleukin-2 pathway
Studies have found that monoclonal antibody complexes consisting of recombinant interleukin-2 (IL-2) and anti-IL-2 monoclonal antibody can preferentially induce the growth and function of regulatory T cells, and thus, can inhibit autoimmune responses associated with autoimmune disorders.
Using the gut microbiota
Studies have found that the content and diversity of the gut microbiota vary between autoimmune patients and healthy individuals. Moreover, it has been found that microbial species that are present in high amounts in autoimmune patients are associated with induction of pro-inflammatory responses; whereas, microbial species that are absent in these patients are associated with induction of anti-inflammatory responses.
Transferring a microbiome from multiple sclerosis patients to germ-free mice has been shown to negatively affect their health. Scientists are trying to modulate the gut microbiota to regulate immune responses and treat patients with autoimmune disorders.
.jpg)
Image Credit: Alpha Tauri 3D Graphics/Shutterstock.com
Further Reading
Last Updated: Aug 20, 2020