Pericarditis is defined as the state of inflammation or infection of the pericardium, the membranous sac that encloses the heart. The cause and severity of pericarditis determines the type of treatment appropriate for this condition.
Pericarditis normally occurs as a mild condition that resolves on its own or through medication with adequate rest. Unless it is associated with complications, interventional procedures are not generally necessary.
The major goals of a specialist in treating this condition are reduction of the inflammation of the pericardium and the pain, finding and curing the root cause, and ruling out further complications.
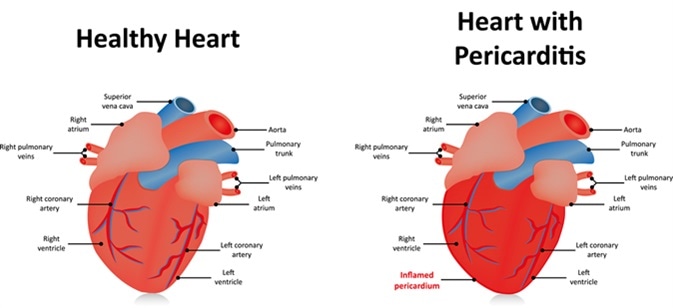
Pericarditis. Image Credit: Joshya / Shutterstock
Nonsteroidal anti-inflammatory drugs
As pericarditis is associated with chest pain and possibly fever, the first line of treatment would be to relieve the pain and resolve the inflammation that is responsible for the fever. Treatment is generally initiated with nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, indomethacin, naproxen, or ketorolac and the patient is advised to rest for about a week or two. This regimen is sufficient to encourage recovery in 70–80% of cases.
If the patient has recently had a heart attack, ibuprofen may be substituted with high-dose aspirin. In some situations, a proton pump inhibitor such as omeprazole or pantoprazole may be added as a protection against gastrointestinal toxicity caused by the NSAIDs in susceptible patients.
If the pain persists and the underlying cause (e.g., an infection) is known, a treatment appropriate to the cause must also be begun. For instance, if tuberculosis or bacterial infection is the underlying cause, the patient may be given appropriate antibiotics. If due to a fungal infection, the patient may require systemic antifungal medication.
Colchicine
For acute or recurrent pericarditis, the patient may be given a drug called colchicine as an adjunct to NSAID therapy. This drug reduces inflammation and the severity of symptoms, as well as decreasing the risk of recurrence.
Although well-tolerated, colchicine has not yet been officially approved for the prevention of recurrent pericarditis in North America and Europe. It is considered unsafe for people who have pre-existing health issues related to the kidney and liver, and also for people who are on certain medications.
Its side effects include abdominal pain, vomiting, and diarrhea.
Corticosteroids
Although the NSAID/colchicine combination is generally safe and effective, some patients may have refractory symptoms. Such patients may require systemic corticosteroid therapy, prednisone often being the drug of choice.
Corticosteroids reduce pericardial inflammation by blocking several immunological pathways. If used for a prolonged duration, they can produce side effects such as weight gain, mood swings, and increased sweating. Thus meticulous monitoring is necessary to ensure that a patient on corticosteroids remains unaffected by steroid toxicity, which can lead to damage to internal organs like the kidneys and the liver.
In a few cases, the use of steroids may even make the condition worse.
Interventional therapies
In some patients with moderate-to-large pericardial effusion which tends to cause or is causing cardiac tamponade, those with significant effusion and recurrent pericarditis, or those with evidence of constrictive pericarditis, medical interventions alone may not be sufficient. In such situations, patients may require some form of percutaneous or surgical intervention as part of their treatment protocol.
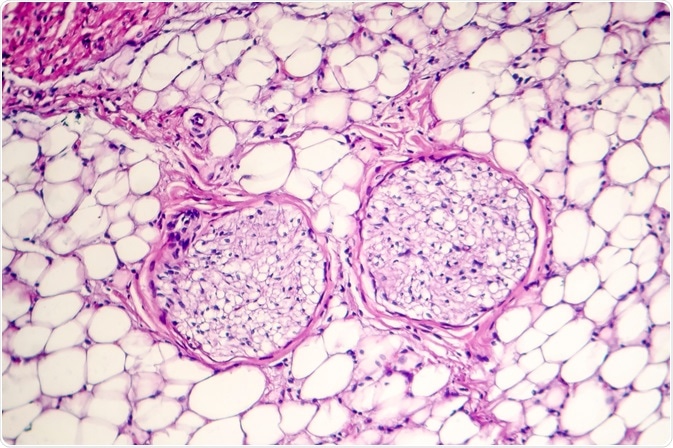 Light micrograph of pericarditus - inflammation in the heart pericardium. Image Credit: Kateryna Kon / Shutterstock.com
Light micrograph of pericarditus - inflammation in the heart pericardium. Image Credit: Kateryna Kon / Shutterstock.com
Pericardiocentesis
Pericardial drainage using a catheter is an effective method to drain the excess fluid out of the pericardial sac and relieve the tamponade. Surgical puncture of the pericardial cavity for the aspiration of fluid is called pericardiocentesis. Catheter drainage may be required for several days at a stretch, and it is generally accepted that the catheter should not be removed unless the daily (24-hr) drainage is less than 20–30 ml. This technique is also useful in reducing the pressure on the heart.
Pericardiectomy
In selected cases, surgical decompression of the pericardium may be attempted either by routine heart surgery or by video-assisted thoracoscopy. This technique, referred to variously as pericardiotomy, pericardiostomy, or window pericardiectomy, is used selectively.
Surgical removal of the entire pericardium (pericardiectomy) is resorted to only when a patient has recurrent pericarditis and is refractory to appropriate medical treatment, or has recurrent cardiac tamponade. It is the definitive mode of management in such cases and has the potential to provide a permanent cure for constrictive pericarditis.
Other techniques
Other less invasive procedures such as balloon pericardiotomy may be used in patients who have reduced life expectancy. The technique involves inserting a balloon catheter into the pericardial space under fluoroscopic or echocardiographic guidance and is quite successful in preventing recurrent effusions.
In any case of pericarditis, medication is generally the first choice of therapy, unless the condition is complex and severe. Although it is not possible to prevent acute pericarditis, one can reduce the chance of recurring episodes by adequate treatment and full compliance with the treatment plan. Full recovery from pericarditis is often achievable provided the patient takes complete rest and has access to ongoing medical care.
References
Further Reading
Last Updated: Dec 9, 2022