Types of arachnoid cysts
Cause and symptoms
Epidemiology
Diagnosis and treatment
References
Further reading
Arachnoid cysts (ACs) are benign, discrete pockets of CSF (cerebrospinal fluid) or CSF-like fluids, accounting for 1% of all intracranial space-occupying lesions. Commonly observed during childhood, ACs can be of two types - primary developmental cysts or secondary cysts.
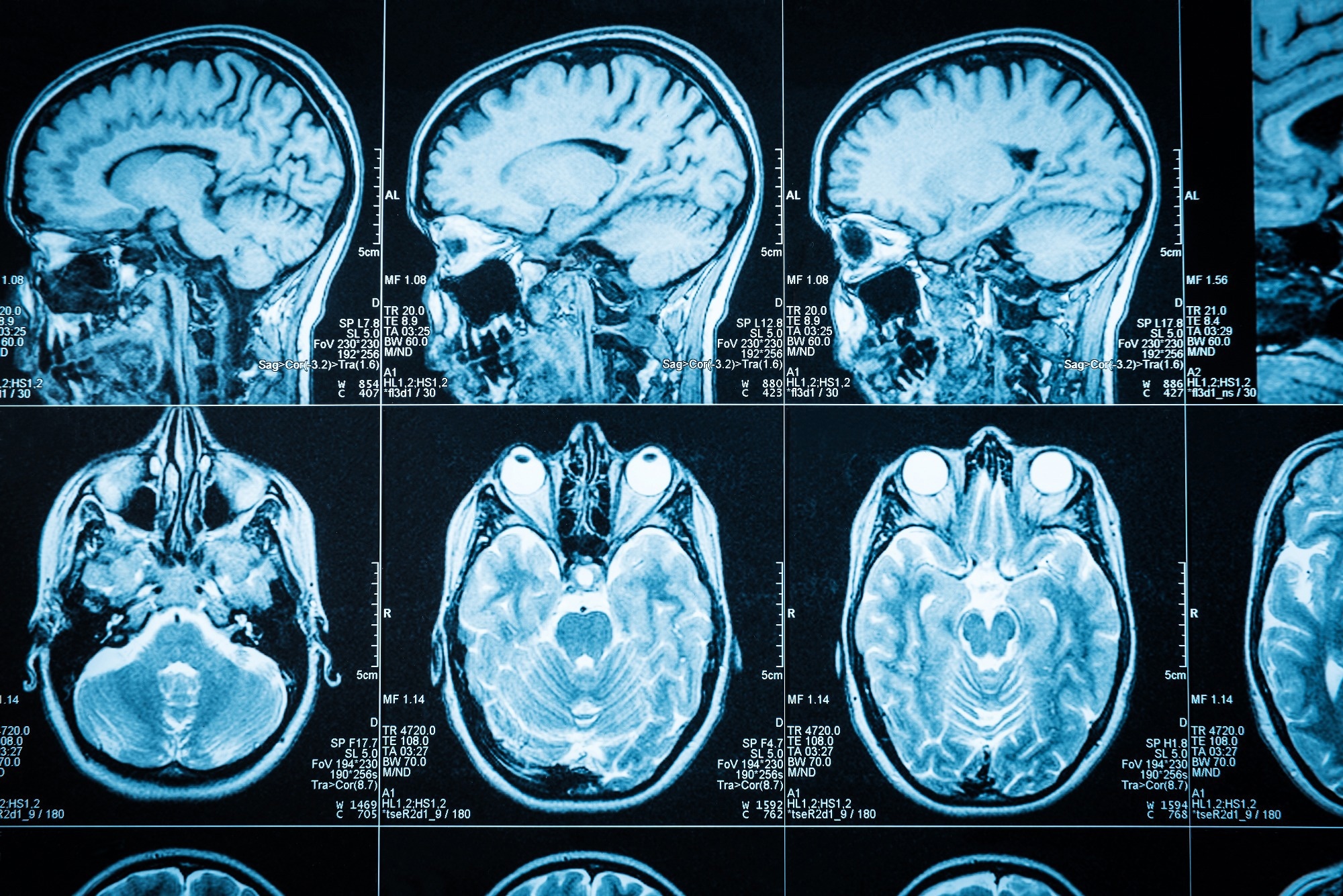
Image Credit: Triff/Shutterstock.com
Common symptoms include headache, dizziness, and vomiting, among others. Arachnoid cyst signs and symptoms differ depending on their size and location.
The underlying mechanisms have been proposed to be congenital, genetic, and traumatic. Around 180 years ago, the first report of cystic abnormalities of the arachnoid layer appeared in the literature.
Types of arachnoid cysts
Primary arachnoid cysts are present at birth and are caused by developmental anomalies in the brain and spinal cord during the first few weeks of pregnancy.
Secondary arachnoid cysts, which occur due to a head injury, meningitis, tumors, or as a complication of brain surgery, are less prevalent than original cysts.
ACs account for 1% of all cerebral space-occupying lesions, with the middle cranial fossa being the most prevalent site. Middle cerebral fossa arachnoid cysts are classified as communicative or noncommunicating intracranial arachnoid cysts based on whether or not they communicate with the circulating CSF.
The Galassi classification method divides middle cerebral fossa arachnoid cysts into three types: type I, type II, and type III. Small spindle-shaped cysts in type one are restricted to the anterior, middle cerebral fossa.
Type II lesions are medium-sized, triangular, or quadrilateral in shape and occupy the anterior and central section of the middle cranial fossa, extending down the Sylvian fissure.
Huge cysts, oval or spherical, almost occupy the middle cerebral fossa and expand toward the hemisphere through multiple regions in type III.
Adult spinal arachnoid cysts (SACs) are uncommon pathogenic entities that frequently manifest as back discomfort or myelopathy. Theories about the pathophysiology of these cysts, such as diverticula in the septum posticum or ectopic arachnoid granulations, have not been proven.
In most cases, no underlying cause for the SAC can be found, and the condition is classified as idiopathic. SACs can develop from arachnoid adhesions caused by trauma, inflammation, or infection in some situations.
Suprasellar arachnoid cysts are typically located near the third ventricle. They are suffering from hydrocephalus. There are two forms of inter-hemispheric cysts: parasagittal and midline. Parasagittal cysts are unilateral, occur in toddlers, and are rarely associated with corpus callosum agenesis. Because these cysts are not near the ventricles, they rarely cause hydrocephalus.
Midline cysts are multiloculated, complicated cysts frequently identified at birth and connected with corpus callosum agenesis. They do exhibit hydrocephalus. The most common point of contact between the cyst and the ventricles is at the third ventricle's roof level.
Only 79 cases of quadrigeminal cistern cysts have been recorded in the literature as of 2008. There are three forms of quadrigeminal cysts. Cysts of Type I have a supratentorial and infratentorial extension, Type II have an infratentorial extension (supracerebellar or supra-retrocerebellar), and Type III has a lateral extension toward the temporal lobe.
Cause and symptoms
The cause of these cysts has not been identified, and various theories have been proposed to explain their development and spread. They are typically extradural but can also be intradural or perineural. There have also been a few reports of intramedullary arachnoid cysts.
Several mechanisms have been postulated to explain their development, including arachnoid membrane splitting or duplication, trauma, and, in some circumstances, genetic considerations.
Some of these cysts grow over time, which has been described variously as fluid entering through one-way valves, fluid discharges by cells lining the cyst lumen, or osmosis. Arachnoid cyst surgical etiologies have also been recorded following various treatments, such as lumbar myelography, laminectomy, and vertebroplasty.
Most patients with arachnoid cysts are asymptomatic; however, in the pediatric population, symptomatic cysts predominate, causing mass effects or hydrocephalus.
Headaches, rapid head growth, developmental delay, early puberty, amenorrhea, seizures, and localized neurologic impairments are all symptoms of arachnoid cysts. Increased intracranial pressure is the most prevalent presenting symptom in children, followed by increased head size, mental developmental delay, and seizures.
Image Credit: peterschreiber.media/Shutterstock.com
Epidemiology
ACs affect people of all ages but are more common in infants and children. Males are four times as likely as females to develop an arachnoid cyst.
In hospital-based and clinical research, a prevalence of 0.5-1.7% was discovered, with men having a two to three times higher frequency than women. Recently, a prevalence of 2.6% in children was reported.
Diagnosis and treatment
The diagnosis is commonly suspected on MRI with focal spinal cord displacement/buckling and, less frequently, on the direct sight of a cystic formation inside the spinal canal with signal patterns comparable to those of CSF.
CT myelography, which may also diagnose the degree of free-flowing CSF between the arachnoid cyst and the main subarachnoid space, can typically provide better delineation.
With the widespread use of MRI, many lesions are now discovered by chance. MRI pinpoints the position and extent of spinal cord compression, but CT myelography (CTM) pinpoints the dural defect through which an extradural cyst communicates with the subarachnoid area.
In symptomatic individuals, good outcomes have been observed following surgery. Surgical exploration and decompression are performed via complete cyst excision, marsupialization, fenestration, communication site ligation, shunting, or a combination of these procedures for managing these cysts.
In the pediatric population, avoiding serious complications associated with major surgery, such as neurologic impairments, subdural hematomas, or hygromas, is critical.
Although shunt insertion may be safer, it carries hazards such as infection, obstruction, and, most critically, lifetime reliance on the shunt, which should not be overlooked.
References
- Sandvik, U., Adolfsson, T., Jacobson, D. N., & Tedroff, K. (2020). Cognition in Children with Arachnoid Cysts. Journal of clinical medicine, 9(3), 850. https://doi.org/10.3390/jcm9030850
- Hall, S., Smedley, A., Sparrow, O., Mathad, N., Waters, R., Chakraborty, A., & Tsitouras, V. (2019). Natural History of Intracranial Arachnoid Cysts. World neurosurgery, 126, e1315–e1320. https://doi.org/10.1016/j.wneu.2019.03.087
- Mustansir, F., Bashir, S., & Darbar, A. (2018). Management of Arachnoid Cysts: A Comprehensive Review. Cureus, 10(4), e2458. https://doi.org/10.7759/cureus.2458
- Fam, M. D., Woodroffe, R. W., Helland, L., Noeller, J., Dahdaleh, N. S., Menezes, A. H., & Hitchon, P. W. (2018). Spinal arachnoid cysts in adults: diagnosis and management. A single-center experience. Journal of neurosurgery. Spine, 29(6), 711–719. https://doi.org/10.3171/2018.5.SPINE1820
- Garg, K., Borkar, S. A., Kale, S. S., & Sharma, B. S. (2017). Spinal arachnoid cysts - our experience and review of literature. British journal of neurosurgery, 31(2), 172–178. https://doi.org/10.1080/02688697.2016.1229747
- Chen, Y., Fang, H. J., Li, Z. F., Yu, S. Y., Li, C. Z., Wu, Z. B., & Zhang, Y. Z. (2016). Treatment of Middle Cranial Fossa Arachnoid Cysts: A Systematic Review and Meta-Analysis. World neurosurgery, 92, 480–490.e2. https://doi.org/10.1016/j.wneu.2016.06.046
- Rabiei, K., Jaraj, D., Marlow, T., Jensen, C., Skoog, I., & Wikkelsø, C. (2016). Prevalence and symptoms of intracranial arachnoid cysts: a population-based study. Journal of neurology, 263(4), 689–694. https://doi.org/10.1007/s00415-016-8035-1
- Al-Holou, W. N., Terman, S., Kilburg, C., Garton, H. J., Muraszko, K. M., & Maher, C. O. (2013). Prevalence and natural history of arachnoid cysts in adults. Journal of neurosurgery, 118(2), 222–231. https://doi.org/10.3171/2012.10.JNS1254
Last Updated: Apr 24, 2023