Skip to:
Varicose veins are enlarged, twisted, swollen veins that are visible under the skin surface. These veins are mostly found in the legs and occasionally cause mild-to-moderate pain, blood clot, and skin ulcer.

Varicose veins on a leg. Illustration Credit: Eyepark / Shutterstock
What are varicose veins?
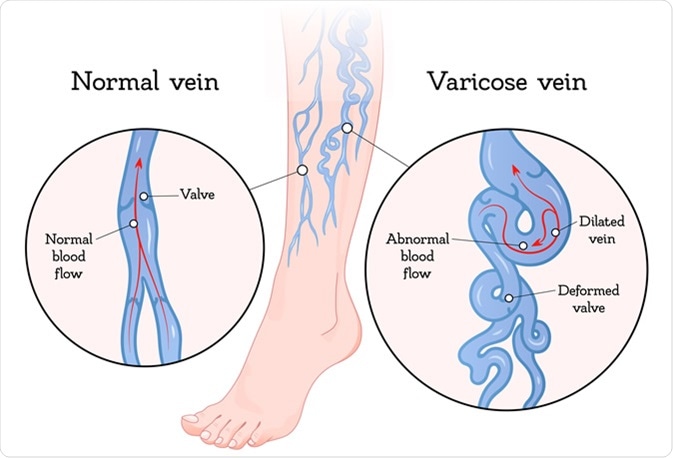
Any damage to the vein valves can lead to varicose veins. Veins that carry deoxygenated blood from the body tissues to the heart contain one-way valves to facilitate unidirectional blood flow. However, backflow of the blood is possible when the valves become weak or damaged, leading to blood pooling in the veins, swelling, and formation of varicose veins.
In general, weakening of the vein walls can potentially lead to loss of elasticity. As a result, vein walls become longer and wider, causing the valve flaps to separate. This subsequently causes blood to flow backward and pool in the veins. Because of the abnormal blood flow, veins become bigger, swollen, and twisted.
Varicose veins illustration. Illustration Credit: VikiVector / Shutterstock
What are the risk factors for varicose veins?
Several factors can increase the risk of varicose veins. The most common risk factor is family history. About 50% of people with varicose veins have affected family members. Moreover, physiological deterioration in old age can also affect the structure and function of the vein valves, leading to varicose veins.
Women are more likely to develop varicose veins than men. Hormonal fluctuations during puberty, pregnancy, and menopause are associated with increased risk. During pregnancy, pressure exerted by the fetus on the leg veins can cause varicose veins. However, the condition gets better within 3 – 12 months of delivery.
People who are overweight or obese also have extra pressure on the leg veins, leading to development of varicose veins. Prolonged sitting or standing with the legs crossed or bent can increase the risk of varicose veins because of lack of blood flow.
Traumatic damages to the vein valves or presence of blood clot can impair the normal functioning of the valves and potentially cause varicose veins.
What are the signs and symptoms of varicose veins?
The most common symptom is dark purple of blue colored veins that are easily visible under the skin surface.
Although mostly not painful, varicose veins sometimes cause mild-to-moderate pain. In such cases, an achy or heavy feeling occurs in the legs. The pain becomes worse after prolonged standing or sitting. Throbbing, cramping, or swelling can also occur in the lower legs. In some cases, the skin around the varicose veins becomes itchy and discolored.
The major complications of varicose veins are dermatitis and superficial thrombophlebitis. Dermatitis often causes bleeding or formation of painful skin ulcers, and thrombophlebitis is formation of blood clot in the veins, causing pain and other problems.
How are varicose veins diagnosed?
In most cases, a physical examination is sufficient to diagnose varicose veins. After checking the affected area, a doctor may ask the patient about signs and symptoms, such as location and intensity of pain.
Sometimes, a doctor also suggests an ultrasound test to check functions of the valves or the presence of blood clot.
How are varicose veins treated?
Varicose veins can be treated with lifestyle changes or medical procedures. If the symptoms are mild, lifestyle changes are sufficient to treat the condition.
Lifestyle changes that are effective in managing varicose veins include:
- Avoid prolonged sitting or standing with the legs crossed or bent. While sleeping, try to raise the legs above the heart level.
- Exercise regularly to improve blood flow and muscle tone.
- Lose weight if you are overweight
- avoid wearing cloths that are tight around the waist, groin, and legs.
- Avoid wearing high heels to improve the tone of the calf muscles.
Besides self-care, doctors also recommend compression stockings to improve the condition. These stockings apply gentle pressure on the legs, which prevents blood pooling and swelling in the legs.
In case of severe varicose veins, doctors recommend different medical procedures to remove or close varicose veins. Common side-effects of these procedures include mild pain, skin discoloration, bruising, and swelling.
Sclerotherapy is used to treat smaller varicose veins. In the procedure, a chemical is injected into the affected vein that causes irritation and scarring inside the vein. This subsequently causes the vein to close and fades away within a few weeks.

Sclerotherapy procedure on the legs of a woman against varicose veins Credit: HENADZI PECHAN / Shutterstock
Foam sclerotherapy is used to treat larger varicose veins wherein a foam solution is injected to form scars and close the vein.
In laser surgery, light energy from a laser is applied onto the varicose veins, which makes the veins disappear slowly. This fully non-invasive surgery is effective in treating smaller varicose veins.
In endovenous ablation therapy, a tiny catheter is inserted into the varicose vein, and the tip of the catheter is heated using radiofrequency or laser energy. The heat is used to destroy and close the vein.
In endoscopic vein surgery, a tiny camera at the tip of a thin tube is inserted to visualize, close, and subsequently remove the varicose vein through small incisions. This technique is used in extreme cases when other procedures fail.
Ambulatory phlebectomy is also used to remove varicose veins that are very close to the skin surface.
High ligation and vein stripping involve tying off a varicose vein and remove it through small incisions.
Further Reading
Last Updated: Sep 17, 2019