Introduction
How artificial intelligence plays a role in MRI
Improvements in PET and CT scans
How image blur is corrected within PET and CT scans
References
Magnetic Resonance Imaging (MRI), computerized tomography (CT) scans, and positron emission tomography (PET) scans have come a long way since their early conception between the 1960s and the 1980s. These non-invasive medical imaging tools have only been enriched since their conception, with artificial intelligence (AI), upgraded methods of raw data acquisition, and multi-parametric statistical methods of analysis all improving how we view and analyze our internal systems.
 Image Credit: Gorodenkoff/Shutterstock
Image Credit: Gorodenkoff/Shutterstock
How artificial intelligence plays a role in MRI
AI has been one of the greatest tools in the hands of medical professionals when it comes to diagnosing and determining which treatments should be used. Adaptive algorithms are foreseen to change the way decision-making is made in medicine.
Robots have been fabricated with the ability to scan a limb or segment of the body and assess the best point of entry. Using ultrasound, blood can now be drawn from the most assessable vein with close to 90% accuracy, circumventing shaky hands and valuable nurse time. This has made the jobs of phlebotomists much easier. AI has also been implemented in other forms of MRI data acquisition, such as Air Recon Deep Learning Software (ARDLS).
ARDLS, developed by GE Healthcare's Edison intelligence platform, encompasses some of the most novel and innovative developments regarding medical imaging. Collecting image noise before and throughout the scan can improve the resolution of every subsequent image. Now available for most clinical scans, this methodology comes with better image quality, better specificity, and a nearly 50% reduction in scan time. It is a deep-learning technology that reduces image noise and ringing from the final reconstruction. An even clearer image can be produced when ARDLS is fit to MRI equipped with 3 Tesla (3.0T) Magnets.
When built into the MRI, the 3.0T magnet can grant a higher spin noise ratio and an improved sharpness or resolution. This is superior to the classic 1.5T MRI. This makes 3.0T MRIs ideal for musculoskeletal, brain, and vascular imaging. However, whether you view it from a physicist’s or a radiologist’s stance, there are some hurdles to improving the quality of MRI and PET scans. It is inherent that, to obtain a better resolution within the scanner, the scan itself will need to be longer, which can lead to patient discomfort, higher energy expenditure, and more time being wasted.
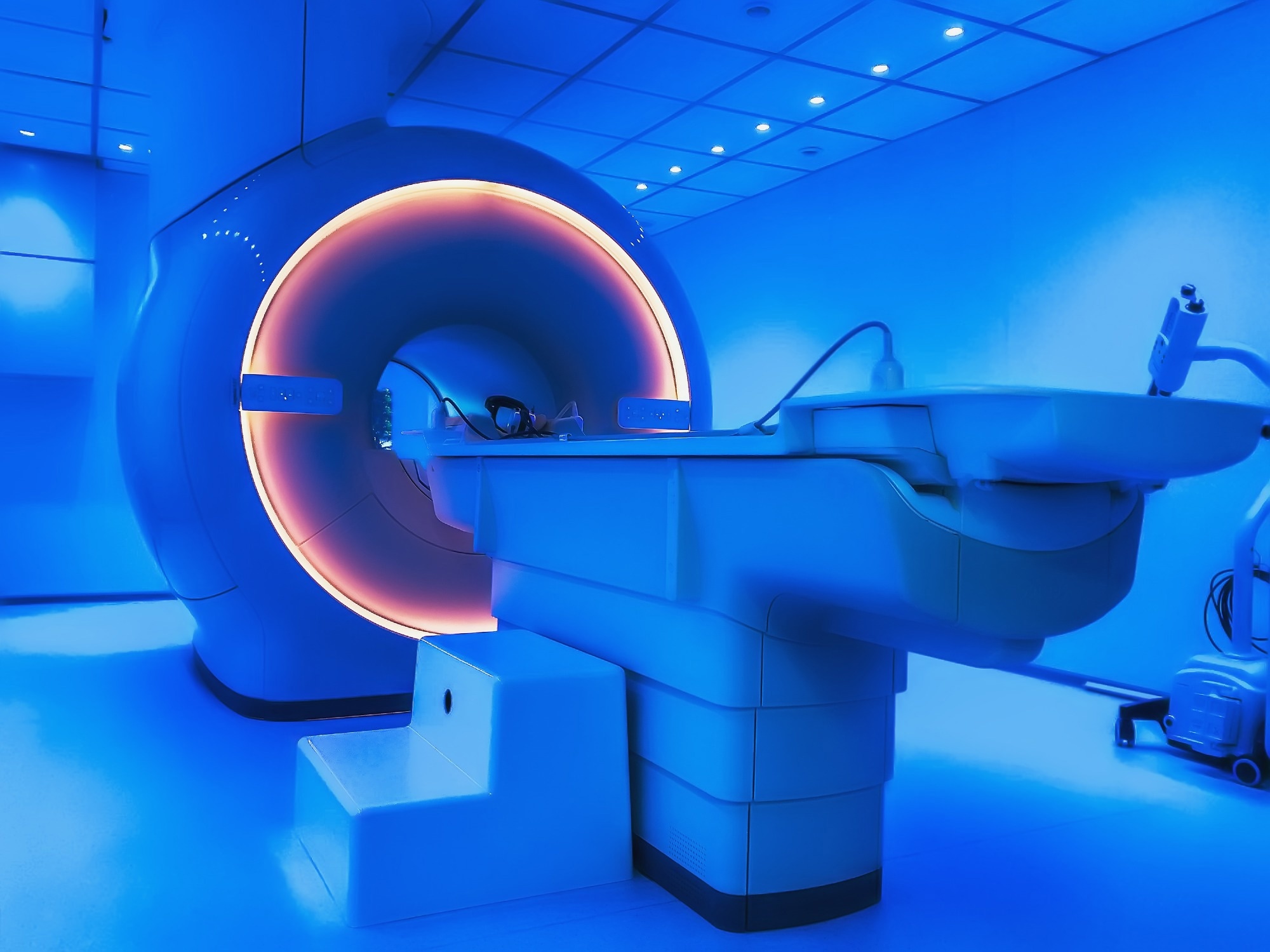 Image Credit: DedMityay/Shutterstock
Image Credit: DedMityay/Shutterstock
Improvements in PET and CT scans
Completing a typical PET scan takes roughly 45 minutes to an hour and can produce clear images of tumor formation amidst the brain, lungs, cervix, and other body areas. Recent developments have only made this technique more useful, implementing software to correct motion blur and allowing algorithmic measures to predict where a mass will be in moving tissue.
A blur occurs if the target segment moves while the PET scan takes an image. This makes assessing and analyzing the mass or tissue much harder. To minimize the amount of motion during the PET scan, healthcare professionals use gated acquisition, which will divide the scanning cycle into multiple “bins.” The program can predict where a target mass will be at a given time or place by segmenting the scanning cycle process into 8-10 bins (depending on user preference). This is done by predicting where the mass was located within the separate bins of a cycle. This gated PET imaging process will, in turn, suppress the motion blur that is inherent in this apparatus. It will improve the activity concentration/standardized update value (SUV). Once the PET data is matched up with CT data, the process as a whole is referred to as 4D CT scanning.
However, there is a known drawback inherent in this process. Image acquisition via gated means does come with greater relative noise because much more data is being acquired. Some approaches to recover from this loss are Q-freeze, Oncofreeze, and time of flight (ToF).
How image blur is corrected within PET and CT scans
Q-freeze image-based correction (using gated type acquisition) involves gathering all images generated and registering them to one another. This registration is done within the image space and gathers all raw data acquired from the PET scan and reconstructs it to generate a final image with limited noise and blur.
OncoFreeze, a mirroring software technique, parallels Q-freeze in some ways, though it is different overall. The motion correction is performed in the sinogram space (raw data space). After acquiring the first image, the subsequent blurred images are projected forward and compared to the surgical work bench projected data and backproject sinogram ratios. This leads to a final updated image based on the deblurred correction image.
Garnering respiratory waveforms in PET scans in conjunction with CT scans, will result in a much better image. By aligning the waveforms of PET scans (a common modus) and the waveforms of CT scans (a newly developed approach), improved alignment can be demonstrated.
References:
- Wang X, Ma J, Bhosale P, Ibarra Rovira JJ, Qayyum A, Sun J, Bayram E, Szklaruk J. Novel deep learning-based noise reduction technique for prostate magnetic resonance imaging. Abdom Radiol (NY). 2021 Jul;46(7):3378-3386.
- Hamill JJ, Meier JG, Betancourt Cuellar SL, Sabloff B, Erasmus JJ, Mawlawi O. Improved Alignment of PET and CT Images in Whole-Body PET/CT in Cases of Respiratory Motion During CT. J Nucl Med. 2020 Sep;61(9):1376-1380. doi: 10.2967/jnumed.119.235804. Epub 2020 Jan 31. PMID: 32005768.
- Huang, T. C., Chou, K. T., Wang, Y. C., & Zhang, G. (2014). Motion freeze for respiration motion correction in PET/CT: a preliminary investigation with lung cancer patient data. BioMed research international, 2014, 167491. https://doi.org/10.1155/2014/167491
- Wood R, Bassett K, Foerster V, et al. (2011) 1.5 Tesla Magnetic Resonance Imaging Scanners Compared with 3.0 Tesla Magnetic Resonance Imaging Scanners: Systematic Review of Clinical Effectiveness. Canadian Agency for Drugs and Technologies in Health; https://www.ncbi.nlm.nih.gov/books/NBK174456/
- Demirel, H. C., & Davis, J. W. (2018). Multiparametric magnetic resonance imaging: Overview of the technique, clinical applications in prostate biopsy and future directions. Turkish journal of urology, 44(2), 93–102. https://doi.org/10.5152/tud.2018.56056
Last Updated: Aug 29, 2023