Deep brain stimulation (DBS) is a neurosurgical procedure that may be used in the treatment and management of Parkinson’s disease, chronic pain, depression, Tourette syndrome and some other health conditions. At this point in time, it is usually reserved for patients that have symptoms that are not adequately responsive to pharmacological treatment.
The procedure involves the implantation of a battery-operated implantable pulse generator that is connected to specific areas of the brain. When activated, this can manipulate the nerve signals in the area and have an impact on the severity of related symptoms.
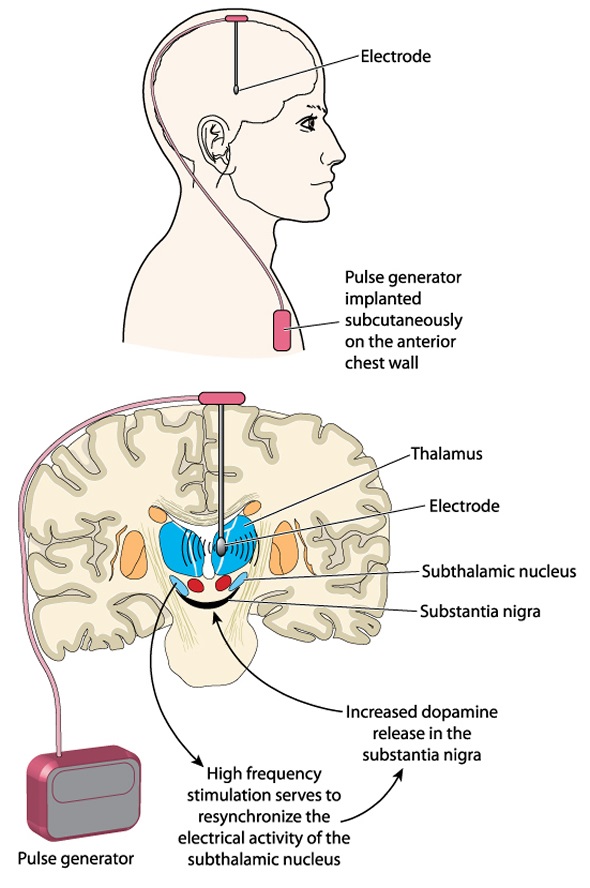
Diagram of deep brain stimulation. Image Credit: Blamb / Shutterstock.com
Pre-Procedure
Prior to the procedure, imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scanning is used to identify the problematic areas of the brain that will be targeting in the treatment. Some neurosurgeons opt to use microelectrode recording that monitors the nerve cells activity to identify the target areas.
For most individuals, the target areas may be in the thalamus, subthalamic nucleus or the globus pallidus.
The System
There are three components of the deep brain stimulation, which are:
- The implanted pulse generator is a neurotransmitter encapsulated in titanium that is used to send electrical impulses into the central nervous system and brain, interfering with the neural activity in specific regions.
- The lead is an insulated coiled wire with platinum-iridium electrodes that are placed into one or two nuclei of the brain to direct the impulses that come from the generator.
- The extension is an insulated wire that is used to connect the lead to the implanted pulse generator, running from the head to the point of entry, which may be as low as the abdomen.
2-Minute Neuroscience: Deep Brain Stimulation
Calibration
The calibration of the system can be conducted by a neurologist, nurse or specialized technician, in a manner to optimize the effect and reduce the risk of side effects.
A local or general anesthetic is usually used while implanting the leads into the brain. A small hole is drilled into the skull, and the electrode lead is inserted stereotactically into the intended area of the brain. If the symptoms are primarily evident on the left side of the body, the lead will be placed on the corresponding right side of the brain and vice versa.
According to the particular health condition and symptoms that are being addressed, the leads are placed near the corresponding regions of the brain. The leads may be placed:
- In the ventrointermediate nucleus (VIM) of the thalamus for essential tremor.
- In the globus pallidus internus or the subthalamic nucleus for dystonia symptoms of Parkinson’s disease (e.g. bradykinesia and tremor).
- In the nucleus accumbens for depression.
- In the posterior thalamic region of the periaqueductal gray for chronic pain.
- In the anterior thalamic nucleus for epilepsy.
There is a small risk of side effects with the placement of the lead for the deep brain stimulation procedure. This may include stroke, bleeding or infection in the brain, usually in the area of the lead placement.
Outcome
Most patients that undergo deep brain stimulation will continue to require medication to manage their symptoms following the procedure. However, the majority of individuals note a significant improvement in their symptoms and the reliance on medications is often reduced.
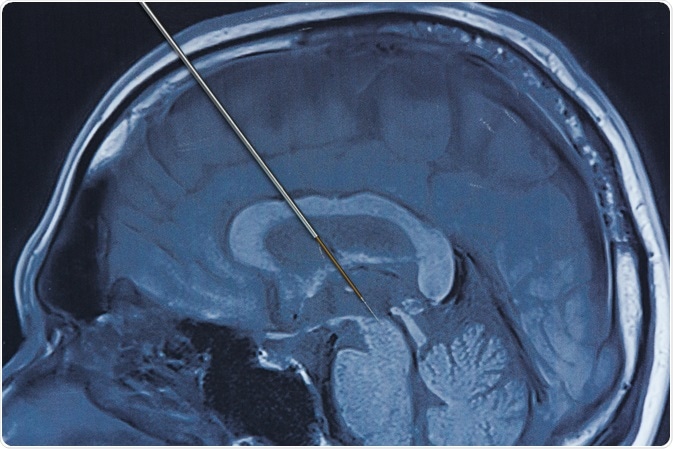 Image Credit: Teeradej / Shutterstock.com
Image Credit: Teeradej / Shutterstock.com
References
Further Reading
Last Updated: Nov 26, 2022