Acute cholangitis is a systemic infection of the biliary system caused by bacterial growth in the bile. Another important cause of the infection is partial or complete obstruction of the bile and/or hepatic ducts.
What is Acute Cholangitis?
Acute cholangitis, also known as ascending cholangitis, is a serious disorder of the biliary system, which can be life-threatening, if left untreated. The most frequent reason of obstruction of the bile or hepatic ducts is choledocholithiasis, which is characterized by the presence of stones in the common bile duct. Other reasons of obstruction include benign or malignant stenosis (abnormal narrowing) of the bile or hepatic ducts, pancreatic cancer, biliary stent obstruction, parasitic colonization in the bile duct, ampullary cancer, porta hepatis cancer, primary sclerosing cholangitis, hepatic amyloid deposition, and strictured bilioenteric anastomoses.
Endoscopic retrograde cholangiopancreatography (ERCP), which is an essential biliary drainage procedure in patients with acute obstructive biliary disorders, may also cause acute cholangitis in some cases. For example, a recent study has shown that exposure to contaminated duodenoscope results in an outbreak of acute cholangitis caused by carbapenem-resistant Enterobacteriaceae bacteria. In addition, the disease has also been diagnosed in about 0.5% to 2.4% of patients who have undergone ERCP.
The average age of acute cholangitis patients is 50 to 60 years. About 6-9% of patients who suffer from gallstone disease (cholelithiasis) are typically diagnosed with acute cholangitis. Since gallstone is one of the main reasons of acute cholangitis, risk factors associated with cholelithiasis such as high fat diet, chronic alcohol consumption, obesity, sedentary lifestyle, and rapid weight loss, may also cause acute cholangitis.
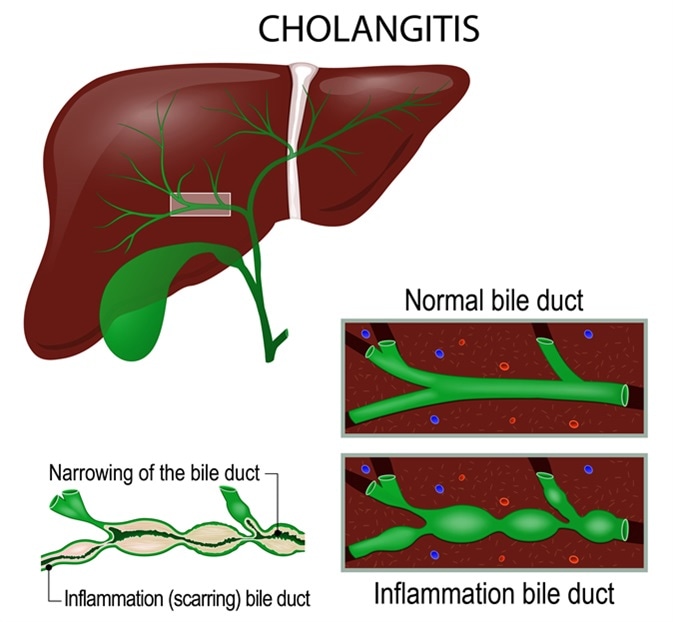
Cholangitis (Ascending cholangitis, acute cholangitis) is an infection of the bile duct. Image Credit: Designua / Shutterstock
Pathophysiology of Acute Cholangitis
One of the important pathological reasons of acute cholangitis is biliary obstruction. In case of unobstructed biliary system, normal bile flow clears any bacterial population that is present in the biliary tract. In addition, bile salts which have bactericidal activity, and biliary epithelium which secretes IgA and mucus, prevent the growth and accumulation of bacteria inside the tract. Biliary epithelium also contains Kupffer cells which prevent the translocation of biliary bacteria into bloodstream.
However, an obstruction within the biliary system hinders normal bile flow, which, in turn, increases the intraductal pressure and causes accumulation of bacteria. An elevated intraductal pressure also increases the bacterial reflux from bile to blood, leading to septicaemia, a fatal complication of acute cholangitis.
The most common bacteria which are known to cause acute cholangitis include Escherichia coli, Klebsiella species, Enterococcus species, and Enterobacter species. In addition, parasitic flatworms such as Clonorchis sinensis, Opisthorchis viverrini, and Opisthorchis felineus; and roundworms such as Ascaris lumbricoides, can also cause acute cholangitis.
Acute cholangitis
Signs and Symptoms of Acute Cholangitis
In 1877, Dr. Jean-Martin Charcot first described acute cholangitis as ‘hepatic fever’. According to his description, common signs and symptoms of acute cholangitis include high fever, right upper quadrant abdominal pain, and jaundice – which are collectively known as ‘Charcot’s triad’. In some severe cases, acute cholangitis is characterized by hypotension and confusion. Although Charcot’s triad is highly specific (95.9%) for acute cholangitis, it has very low sensitivity (26.4%).
To establish a more effective and sensitive diagnostic guideline, TG07 diagnostic criteria for acute cholangitis were prepared at the International Consensus Meeting, Tokyo, in 2006. According to TG07, diagnostic parameters include history of biliary disease, fever and/or chills, jaundice, abdominal pain, inflammation, abnormal liver functions, and biliary dilatation or evidence of an etiology (stone, stricture, stent, etc.). In 2012, a new Tokyo guideline, TG13, was prepared to diagnose acute cholangitis.
Diagnosis of Acute Cholangitis
The diagnosis mainly includes laboratory tests such as complete blood count, erythrocyte sedimentation rate, metabolic profiling, etc. Imaging analyses include abdominal ultrasound, computed tomography, magnetic resonance cholangiopancreaticography, and endoscopic ultrasound (EUS).
Management of Acute Cholangitis
The treatment of acute cholangitis mainly includes systemic antibiotic therapy and biliary drainage techniques. The choice of antibiotics depends on many factors such as patient’s metabolic profile, drug allergy, presence of other disorders/infections, and severity of acute cholangitis. Both Gram-negative and anaerobic organisms should be considered, while selecting the antibiotics.
Regarding biliary drainage techniques, the most frequent and effective one is ERCP. Other techniques include endoscopic nasobiliary drainage (ENBD), percutaneous trans-hepatic biliary drainage (PTBD), EUS-guided drainage, and open surgical drainage (T-tube drainage after laparotomy).
Reviewed by HH Patel, M.Pharm.
Further Reading
Last Updated: Oct 8, 2018