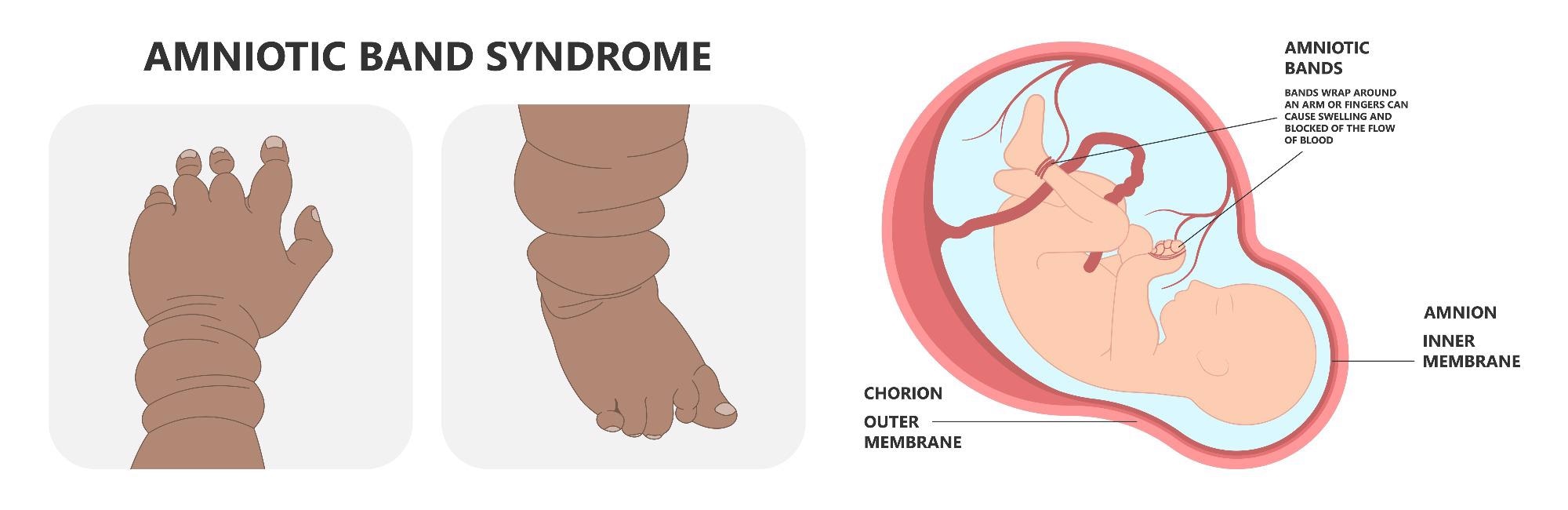
Amniotic band syndrome (ABS), also known as congenital constriction ring or constriction band syndrome is a rare condition comprising several different abnormalities.

Ultrasound of human fetus. Image Credit: AePatt Journey/Shutterstock.com
During pregnancy, the lining of the amniotic sac gets damaged leading to amniotic band syndrome. Due to this, the tissues divide and form string-like structures called strands that entangle the fetus and other developing parts of the body. As a result, blood flow is constricted.
This prevents the fetus from growing correctly by constricting blood flow and results in a variety of birth abnormalities. Amniotic band syndrome can range in severity from a single, isolated issue to several, disfiguring sequelae. Arms and legs are the most commonly affected areas of the body.
Causes
ABS has no known cause, however, researchers have ruled out genetics as a possible cause. It usually occurs when the amniotic sac lining is ripped during pregnancy. Amniotic band syndrome is influenced by a complex and controversial set of mechanisms.
The complicated mechanisms that underpin amniotic band syndrome have been the subject of several theories. The extrinsic theory and the intrinsic theory are the two basic theories. The extrinsic theory claims that amniotic band syndrome is caused by variables outside of the fetus (externally); the intrinsic theory states that amniotic band syndrome is caused by factors inside the fetus (internally).
The specific cause of tears or ruptures of the amniotic sac is not always known, and researchers believe that it may occur at random in some circumstances. Specific environmental influences have been discovered in some situations. In some cases, ABD seemed to have originated as a result of abdominal trauma (during pregnancy) and placental blunt trauma.
A small number of babies are damaged by the diagnostic technique chorionic villus sampling (CVS) when used early in pregnancy. Amniotic band syndrome has also been observed as a result of strong uterine contractions caused by the drug misoprostol (a prostaglandin E1 analog used to treat gastric ulcers).
Symptoms
The symptoms of amniotic band syndrome differ widely from one baby to the next. Some babies are born with only minor deformities, while others are born with severe and even life-threatening defects. The symptoms of amniotic band syndrome appear to occur largely in the first 12 weeks of pregnancy (first trimester). Damaged limbs, craniofacial abnormalities, problems of the brain, and significant malformation of the arms and legs are the three most prevalent forms of amniotic band syndrome.
The majority of infants with amniotic band syndrome have deformities in their arms and legs, as well as their fingers and toes. One or more limbs may be afflicted. The upper limbs are more commonly damaged than the lower limbs. ABD may lead to the formation of a minor dent around a finger or limb.
Deeper bands, on the other hand, can cause major swelling, shut off blood supply, or prevent that region of the body from growing properly. If a band is too tight, it can result in amputation in utero (before delivery).
The type of malformation caused by ABS is determined by the area of the body involved. Atypical clefts of various types, including those affecting the eyes, nose, and ears, may develop if it affects the orofacial region. Constriction rings, amputations, aberrant dermatoglyphs, pseudo syndactyly, and clubbed feet are among the limb anomalies.
Anencephaly, encephalocele, asymmetrical microphthalmia, nasal deformities, cleft lip and palate, and aberrant calcification of the skull are all craniofacial anomalies associated with ABS. The most prevalent visceral abnormalities are omphalocele and gastroschisis.
Epidemiology
Amniotic band syndrome is thought to affect 1 in every 1,200 to 15,000 live births. There are no known gender or racial predispositions to amniotic band syndrome. Boston hospital conducted a long-term observation of nearly 300,000 births. A total of 40 infants (1 in every 7,500) born with amniotic band syndrome were identified through this observation.
Amniotic band syndrome. Image Credit: rumruay/Shutterstock.com
Diagnosis and treatment
The amniotic bands are difficult to identify on a regular ultrasound and thus, ABS is usually diagnosed at delivery. Doctors usually recommend the patients to a fetal clinic to confirm the diagnosis.
Anatomy ultrasound (to confirm the diagnosis, determine where the bands are placed, and measure blood flow), MRI (to check the severity of constriction and anomalies), and fetal echocardiography (to examine the baby's heart structure and function) are some of the other diagnostic tests available. These techniques give more information and photographs regarding your baby's condition.
In some situations, the disorder can be suspected before birth (prenatally). This is attributed to the results of specialist imaging techniques such as fetal ultrasonography, which can indicate typical malformations. The image of the developing fetus is created using reflected high-frequency sound waves during fetal ultrasonography.
After the diagnosis, regular monitoring is done to keep a check on the growth and development of the baby. Regular ultrasounds help in identifying possible risks and facilitate the development of a care plan. Treatment usually involves supportive therapies and care.
Mild birth abnormalities may not necessitate medical intervention. However, in severe cases, some infants may require medical or surgical intervention. Babies may require surgery immediately after birth or later in life.
When necessary, emergency surgery to remove the restricting bands is performed. Plastic and reconstructive surgery to correct defects may take months or even years to complete to allow the infant to develop normally. Rehabilitative therapy (physical and occupational) can be used on some infants to help them gain strength and function.
Reference:
Further Reading
Last Updated: Mar 21, 2022