Asherson’s syndrome, also known as catastrophic antiphospholipid syndrome (CAPS), is an extremely rare autoimmune condition. It is defined by the fast progression of blood clots impacting many organ systems of the body over hours, days, or weeks. Infections, vaccinations, wounds caused by physical trauma, and failure of the body's anticoagulation mechanism are all examples of "triggers."
Patients with antiphospholipid syndrome who encounter a stop of the anticoagulation mechanism as a result of repeated bleeding in the body are more likely to develop the syndrome. Patients who have previously experienced a simple/classic episode of the antiphospholipid syndrome are more likely to develop this condition.
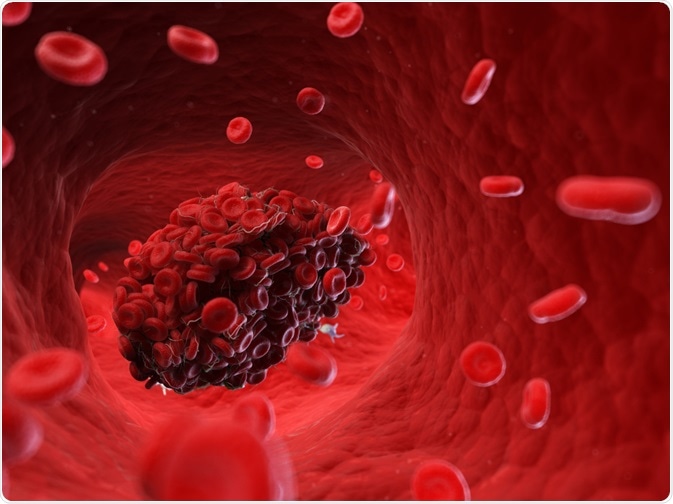
Image Credit: SciePro/Shutterstock.com
Causes of asherson’s syndrome
An autoimmune condition develops when the body's natural defenses (antibodies, lymphocytes) against invading pathogens suddenly begin to target perfectly healthy tissue. According to researchers, multiple factors like genetic and environmental have a role in the development of autoimmune illnesses.
Antiphospholipid syndrome, also known as Asherson's syndrome, is defined by the presence of certain antibodies in the body and the formation of blood clots. Antiphospholipid antibodies (aPL) are antibodies that are present in both antiphospholipid syndrome and Asherson's syndrome.
Individuals with primary or secondary antiphospholipid syndrome may develop Asherson's syndrome. It can also happen to those who have never had these problems before. The cause of the syndrome is uncertain. In some cases, researchers have discovered a precipitating event, or "trigger," that contributes to the formation of the numerous blood clots that characterize this illness.
Infection is the primary cause. Trauma, such as that induced by invasive surgical operations, the discontinuation of anti-clotting medication, pregnancy, and some underlying malignancies, are additional factors (cancers).
Symptoms
Complications resulting from the development of numerous blood clots (thromboses) in the body generate the symptoms of Asherson's syndrome. Multiple blood clots can form in hours, days, or weeks, posing a life-threatening risk of multiorgan failure.
Depending on which organ systems are implicated, specific symptoms differ. Commonly afflicted organs include the kidneys, stomach, lungs, heart, skin, and central nervous system. Renal involvement can lead to kidney dysfunction and symptoms such as decreased urine output and high blood pressure (hypertension).
Blotchy reddish areas of discolored skin (livedo reticularis), bruising, and the loss of living tissue (gangrene) are possible side effects. Stroke (cerebral infarction), seizures, and a disorder characterized by altered brain structure and function are examples of symptoms related to the central nervous system(encephalopathy). If the heart is affected, symptoms may include heart valve inflammation and thickening (valvar heart disease), leading to complications including mitral valve regurgitation (MVR). Individuals who are affected may also experience chest pain (angina) and the risk of a heart attack (myocardial infarction).
Additional organ systems that may be affected by this syndrome are the gastrointestinal system (abdominal pain and cramping), the bone marrow (anemia and thrombocytopenia), and the adrenal and pituitary glands (hormone imbalances and low blood pressure).
Epidemiology
Since the condition was originally described in the medical literature in 1992, over 300 people have been diagnosed with Asherson's syndrome. Women have been impacted more than males. Although the illness can affect anyone at any age, the majority of cases have been observed in young people.
Significance in obstetric complications
The function of CAPS in the pathophysiology of obstetric problems has gotten a lot of attention in recent years. APS is a systemic condition that affects all of the body's organs and tissues.
The placenta is the most crucial organ during pregnancy. Preeclampsia, HELLP syndrome, and placental abruption are all maternal problems caused by placental function violations caused by endothelial dysfunction, ischemia, and placenta microthrombosis. The presence of these problems in APS patients is always a warning sign for CAPS. The presence of aPL is thought to increase the risk of preeclampsia.
Diagnosis
A thorough clinical evaluation, identification of characteristic findings (e.g., multiple blood clots affecting at least three different organ systems that appear simultaneously within one week), and a variety of tests, including simple blood tests that detect antiphospholipid antibodies, are used to diagnose Asherson's syndrome. A coagulation test is a specialized blood test that measures blood clotting and can detect the presence of lupus anticoagulant in the blood.
Anticardiolipin antibodies can be detected in the blood using an Enzyme-Linked ImmunoSorbent Assay (ELISA). Antiphospholipid antibodies can be present for brief periods (transiently) due to other factors such as infection or drug use, hence positive tests may need to be repeated frequently. Because many with APS had first tested negative for antiphospholipid antibodies, borderline negative testing may need to be redone.
Classification
It is necessary to standardize the CAPS diagnostic criteria to facilitate diagnosis and assure the best possible early start of therapy. Multiple thromboses developing in a short period (less than a week), multiorgan failure, thrombosis in small vessels, a high risk of abnormal thrombosis (bone marrow and reproductive organs), development of Systemic inflammatory response syndrome (SIRS), and laboratory signs of APS are included in the modern definition of CAPS.
Treatment
Due to its recent identification and a limited number of cases, no conventional therapy for Asherson's syndrome has been approved. Anticoagulants, corticosteroids, specific proteins (immunoglobulins), and frequent plasma exchanges (using the plasmapheresis method) are the therapy regimens recommended by researchers who have studied the condition. Individuals are usually treated with the anticoagulant heparin, administered intravenously. Heparin and corticosteroids may be given together. Steroids are used to reduce the consequences of tissue loss (necrosis), a common side effect of the syndrome.
Infection may be treated with intensive antibiotic therapy. More research into the long-term impact of Asherson's syndrome is needed, however, doctors examining the condition have found that those who survive the early start of many blood clots have a good prognosis.
Future therapies have enormous possibilities, but they will require the active participation and collaboration of many clinicians around the world, especially those working in intensive care units.
References:
- Arakelyan, H., S., & Forghanisardaghi M. (2019). Asherson's Syndrome-Catastrophic Antiphospholipid Syndrome. Rare Autoimmune Diseases.
- Makatsariya, A., Khizroeva, J. & Bitsadze, V. (2018). Catastrophic antiphospholipid syndrome (Ronald Asherson syndrome) and obstetric pathology. Journal of Perinatal Medicine, 46(4), 387-400. https://doi.org/10.1515/jpm-2017-0092
- Cervera, R., & Asherson, R, A. (2008). Catastrophic antiphospholipid (Asherson's) syndrome. British Journal of Hospital Medicine, 69(7), 384–387. doi: https://doi.org/10.12968/hmed.2008.69.7.30413
- Asherson R. A. (2006). The catastrophic antiphospholipid (Asherson's) syndrome. Autoimmunity reviews, 6(2), 64–67. https://doi.org/10.1016/j.autrev.2006.06.005
- Asherson’s Syndrome. [online]. National Organizations for Rare Disorders. Available at: https://rarediseases.org/rare-diseases/ashersons-syndrome/
Further Reading
Last Updated: Nov 19, 2021