Atresia, a congenital birth defect, is a leading cause of bowel obstruction in newborns. The membrane that connects the small intestines to the abdominal wall is partially or completely absent in patients. This causes twisting of the jejunum around an artery supplying blood to the colon. The marginal artery results in intestinal blockage, commonly known as atresia.
The distal small bowel comes directly off the caecum and bends around the marginal artery due to agenesis of the mesentery in this disease, resembling a maypole, a Christmas tree, or an apple peel during operation. It is also referred to as apple peel syndrome or apple peel small bowel syndrome.
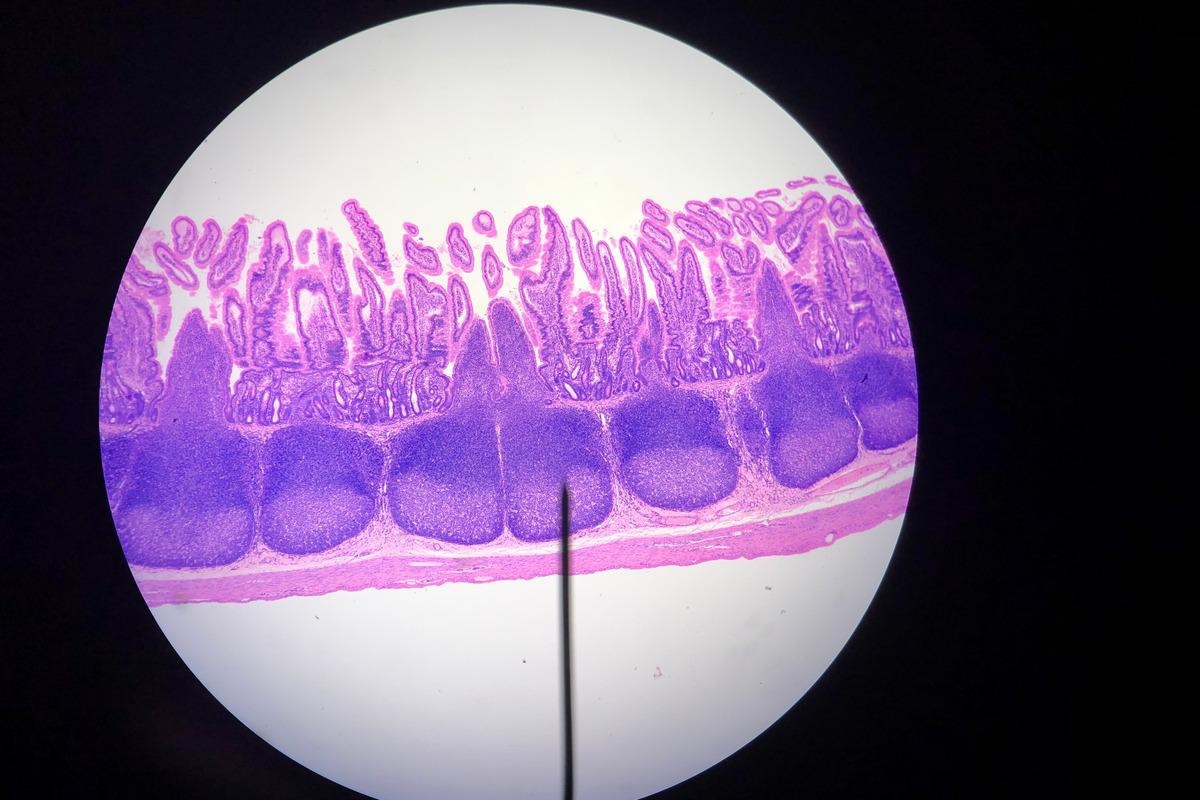 Image Credit: Karakirky/Shutterstock
Image Credit: Karakirky/Shutterstock
Intestinal artesia
The terminology "intestinal atresia" refers to a variety of congenital abnormalities that cause a blockage in either the small or large intestine. The intestines stay unobstructed during normal fetal growth, allowing stomach contents to move smoothly through the baby's digestive tract.
However, the intestines lose part or all of their ability to absorb nutrients and pump food and fluids through the baby's digestive tract when a blockage occurs.
The different types of intestinal atresia are duodenal atresia, jejunal atresia, ileal atresia, and colonic atresia. A blockage of the upper section of the small intestine, or duodenum, causes duodenal atresia. It is caused by a different disease mechanism than other forms of intestinal atresia, and it is sometimes linked to other birth abnormalities. Ileal atresia is an obstruction in the ileum, the small intestine's final and longest part, whereas colonic atresia is a blockage in the large intestine or colon.
Cause and symptoms
The membrane that connects the small intestines to the abdominal wall (known as the mesentery) is partially or entirely missing in jejunal atresia. The jejunum coils around the marginal artery as a result. This causes an obstruction in the intestine, known as "atresia." Scientists believe it's caused by an interruption in blood flow in the growing fetus, which causes cells and tissue in the affected area to undergo necrosis. There are a variety of reasons why blood flow is disturbed.
Because jejunal atresia affects only a few members of a family, it's possible that there's a genetic component or susceptibility in some situations. The majority of occurrences of jejunal atresia occur in people who have no family history of the disorder. It rarely affects more than one family member, though. Jejunal atresia appears to be inherited in an autosomal recessive or multifactorial fashion in these families, indicating that it is likely attributable to a genetic etiology.
Signs and symptoms of jejunal atresia can vary from patient to patient. These include feeding difficulties, vomiting bile, abdominal swelling (especially in the upper-middle part exactly below the breast bone), absence of bowel movements after birth, and failure to thrive.
There are 4 types of jejunal atresia – Type 1, type 2, type 3, and type 4, and male and female neonates are equally affected by jejunal atresia.
Case reports
In 2021, Hyun Nam et al. reported a 1-day-old female child was referred to a hospital with bilious vomiting. The baby was delivered at 39 weeks gestational age and weighed 3,320 grams at delivery. At 1 minute, the Apgar score was 9, and at 5 minutes, it was 10. During the antenatal checkup, her mother was a 35-year-old primiparous lady with no history of polyhydramnios. On physical inspection, the infant appeared to be in good health and appeared to be completely normal. There was no abdominal distension or redness, and the anus was opened in the correct spot.
Following jejunal intussusception induced by a 2.5-cm intraluminal mass, a type I jejunal atresia was discovered. The infant recovered without complications after a little intestinal resection and anastomosis. Histological examination revealed that the tumor was a heterotopic pancreas. The stool cleared two days after surgery, and milk feeding began five days afterward.
Galani et al., in 202, described the case of a 33-week-old fetus who was diagnosed with jejunal atresia. At 33 weeks of pregnancy, a 35-year-old pregnant lady was brought to the hospital's emergency department with vaginal fluid leakage. So far, her pregnancy had been low-risk. She didn't use any regular medications, had no known allergies, and didn't smoke. Preterm rupture of membranes was diagnosed after a vaginal speculum examination indicated amniotic fluid flow from the cervical os. A normal-sized fetus was discovered during a transabdominal ultrasound. The deepest vertical pool measured 10 cm, indicating polyhydramnios. Small intestinal dilatation was also observed, with a maximum diameter of 25 mm.
These findings fit the description of fetal jejunal atresia. There were no further fetal anomalies discovered during the ultrasound. The parents were given comprehensive information about the diagnosis of fetal intestinal atresia, the potential for further anomalies, and postnatal care and prognosis. She delivered a female newborn weighing 2,680 g by cesarean section at 34+5 weeks of pregnancy.
According to the neonatal team's recommendations, the newborn received X-ray imaging, and surgical management verified the diagnosis of jejunal atresia. A total of 70 cm of the jejunal was revealed to have several atresias. After the diagnosis was confirmed, the complete small bowel portion was removed and an end-to-end anastomosis was performed. After the operation, the infant's condition was outstanding, and she was discharged three weeks later.

Image Credit: Gorodenkoff/Shutterstock
Diagnosis and treatment
Jejunal atresia can sometimes be detected before birth using a prenatal ultrasound or fetal MRI. This is advantageous since infants can be treated as soon as they are born, minimizing the likelihood of problems. X-rays and imaging examinations with contrast should be conducted after birth to confirm the diagnosis because prenatal ultrasonography may not always be reliable.
A diagnosis is frequently suspected after birth based on the presence of specific signs and symptoms that suggest intestinal obstruction. Abdominal distension, bile vomiting, and a failure to pass stool are all possible symptoms. The diagnosis can then be confirmed using imaging investigations.
Surgery is usually used to cure jejunal atresia as soon as possible. Following surgery, total parenteral nutrition (TPN) is usually required for a period of time until normal meals can be tolerated. Patients and their families may seek genetic counseling as well.
References:
- Nam, S. H., & Han, S. H. (2021). Jejunal atresia due to heterotopic pancreatic intussusception. Journal of Pediatric Surgery Case Reports, 66, 101805. https://doi.org/10.1016/j.epsc.2021.101805
- Galani, A., Zikopoulos, A., Papandreou, L., Mastora, E., Zikopoulos, K., & Makrydimas, G. (2021). Prenatal Diagnosis of Fetal Jejunal Atresia: A Case Report. Cureus, 13(10), e18947. https://doi.org/10.7759/cureus.18947
- Marei, M. M., Abouelfadl, M. H., Rawwash, A. A. E., Seleim, H. M., Mahmoud, W. M., Yassin, T. Y. M., & El-Tagy, G. H. (2019). Early outcomes of tapering jejunoplasty by antimesenteric seromuscular stripping and mucosal inversion for proximal jejunal atresia. Egyptian Pediatric Association Gazette, 67(1), 1-7. https://doi.org/10.1186/s43054-019-0003-9
- What is intestinal atresia? [Online] Children’s Minnesota - MIDWEST FETAL CARE CENTER. Available at: https://www.childrensmn.org/services/care-specialties-departments/fetal-medicine/conditions-and-services/intestinal-atresia/
- Jejunal atresia. [Online] NIH-GARD. Available at: https://rarediseases.info.nih.gov/diseases/6799/jejunal-atresia
- Jejunal Atresia. [Online] National organization for rare disorders. Available at: https://rarediseases.org/rare-diseases/jejunal-atresia/#:~:text=Jejunal%20atresia%20is%20a%20rare,of%20the%20proximal%20small%20intestine.
Further Reading
Last Updated: May 19, 2022