Cases of a rare and difficult to treat “black fungus” are rising in COVID-19 patients in India due to the increased use of steroids like dexamethasone. Known as Mucormycosis, the infection is highly serious and has a high mortality rate. With more than 300 cases being reported in four Indian cities at the beginning of May, there is increasing concern about the risk to public health, particularly to those who are vulnerable.
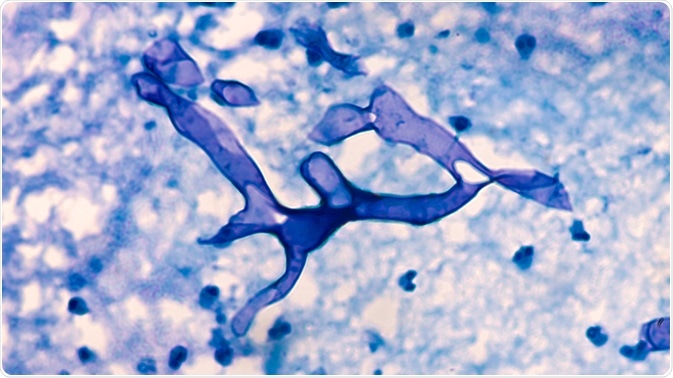
Mucormycosis. Image Credit: David A Litman/Shutterstock.com
What is Mucormycosis?
Mucormycosis is an incredibly rare infection caused via exposure to a group of molds called mucormycetes that are found in the environment: manure, plants, soil, and organic decaying matter such as fruits and vegetables are all sources of mucormycetes, such as the mucor mold. It is often found in the soil and air and even in the nasal passages and mucus of healthy people.
However, exposure to the mold alone rarely causes infections, usually, infections occur in those who are severely immunocompromised, such as patients underling cancer therapy and those with HIV/AIDS. It is also life-threatening in those with diabetes. In those who are vulnerable, the microscopic fungal spores of the mucormycetes can infiltrate the sinuses, the brain, and the lungs, causing an infection that can spread to other tissues.
Mucormycosis has a range of symptoms, depending on where the infection has developed. Symptoms of mucormycosis of the sinus and brain, known as rhinocerebral mucormycosis, include one-sided facial swelling, headache, nasal or sinus congestion, black lesions on nasal bridge or upper inside of the mouth, and fever. Symptoms of pulmonary (lung) mucormycosis include chest pain, cough, fever, and shortness of breath.
Mucormycosis can also infect the skin, particularly, it can infiltrate cuts and wounds. Symptoms of cutaneous (skin) mucormycosis include blisters and ulcers on the skin, pain, warmth, and excessive redness and swelling around the wound. Finally, symptoms of gastrointestinal mucormycosis include abdominal pain, gastrointestinal bleeding, nausea, and vomiting.
The prognosis for those diagnosed with mucormycosis is poor, it is often life-threatening and has an incredibly high mortality rate. Recent research estimates that it has an overall all-cause mortality rate of 54%. The evidence indicated that mortality rate was influenced by factors such as the type of fungus responsible for the infection, the body site infected (mortality rate by infection site: 46% for sinus infections, 76% for pulmonary infections, 96% for disseminated mucormycosis).
Mucormycosis and COVID-19: a nightmare inside of a pandemic
In light of the current rise in mucormycosis in COVID-19 patients in India, Prof Peter Collignon, who is active on the World Health Organization’s expert committee on antibiotic resistance and infectious diseases, has stressed that the infection is “is very serious, has a high mortality, and you need surgery and lots of drugs to get on top of it once it takes hold”. The healthcare system in India urgently needs to respond to the situation to protect the lives of the increasing number of people who have been infected with COVID-19.
While mucormycosis is a rare infection, unfortunately, the COVID-19 pandemic is creating conditions to allow the infection to thrive. Often, to treat COVID-19, patients are given high-dose steroids to treat the inflammation that is characteristic of COVID-19, however, it also surpasses the immune system, making the body vulnerable to other infectious pathogens. In India, cases of mucormycosis are particularly being seen in those with diabetes, a condition that also lower’s the body’s natural immune defenses.
This double-drop in immunity is what is thought to have triggered the surge in mucormycosis in India, where crowded and cramped conditions are giving the pathogen a better chance to take hold. Sion Hospital, based in Mumbai, has reported 24 cases of mucormycosis in the last two months, up from just six cases being reported on average each year at the hospital.
Of the 24 patients who were diagnosed with mucormycosis, six of them died, and one lost an eye to the infection. Mostly, patients had recently recovered from COVID-19 and had diabetes. Dr. Renuka Bradoo, head of the ear, nose, and throat wing at Sion hospital called it a “nightmare inside a pandemic”. Other hospitals have reported patients losing their vision in both eyes, and in some cases, patients have had their jaw bone surgically removed to prevent the infection from spreading.
The clear message coming from doctors who have experienced treating patients with mucormycosis is that patients are arriving too late when they have already begun to lose vision. On Sunday, 9th May, the Indian Council of Medical Research and India's Health Ministry issued an advisory addressing the rise in mucormycosis cases, calling for an increased awareness of the disease, as well as for better screening and management. The advisory will hopefully lead to greater awareness of the disease in the medical community, where many doctors have not seen many, if any, cases.
Further Reading
Last Updated: May 20, 2021