Introduction
Causes and symptoms
Epidemiology
Ollier disease and Maffucci syndrome
Case reports
Diagnosis and treatment
References
Further reading
Ollier disease (OD) is a rare, nonhereditary benign bone disease. Multiple enchondromatosis with a typical asymmetrical distribution restricted to the appendicular skeleton is the characteristic feature of OD. The development of an enchondroma into chondrosarcoma is the most dangerous complication of OD.
Ollier originally defined the disease as an uncommon condition characterized by numerous unilateral limb endogenous chondromas with limb abnormalities in 1889. The clinical signs of this disease are more common in the first ten years of life. Ollier disease has a difficult prognosis.
 Image Credit: Darya Komarova/Shutterstock
Image Credit: Darya Komarova/Shutterstock
Causes and symptoms
Although it has been suggested that the incidence of Ollier disease may be associated with somatic mosaic mutations of isocitrate dehydrogenase IDHI and IDH2, the etiology of the disease has yet to be proven. It was also proposed that somatic mutations in the parathyroid hormone 1 receptor (PTHR1) (R150C) gene may be linked to the onset of Ollier disease. These two theories argue that the disease is a non-hereditary disease; it is a non-familial genetic disease that develops spontaneously and is not passed down through the generations. Although the disease's etiology has been identified, the pathogenesis is yet to be fully understood.
Local discomfort, bone swelling, and palpable bony masses are common clinical symptoms in the first decade of life and are frequently associated with bone malformation. Clinical findings include headache and cranial nerve palsy. Enchondromas on the extremities are frequently apparent as lumps implanted inside the phalanges, metacarpal, and metatarsal bones on physical examination. Long tubular bones, such as the tibia, femur, and/or fibula, are usually afflicted by enchondromas; flat bones, particularly the pelvis, can also be impacted. The lesions can affect numerous bones and are frequently asymmetrically distributed, affecting one side of the body solely or predominately. Bones that have been affected are frequently shorter and misshapen.
Shortenings of the bones are frequently coupled with bending and curving of the bones, which can impede articular movement. Deformities of the forearm are very common. In Ollier illness, the reported incidence of malignant transformation of enchondromas ranges from 5% to 50%, with one multicenter study reporting a rate of 40%. Between the ages of 13 and 69, malignant transformation is most common. Intracranial lesions have previously been described, and astrocytoma (low-grade to glioblastoma multiforme) and oligodendroglioma are the most common types of CNS cancers linked with Ollier syndrome.
Epidemiology
The prevalence of Ollier disease is estimated to be 1 in every 100,000 people. No gender-related trends have been reported to date.
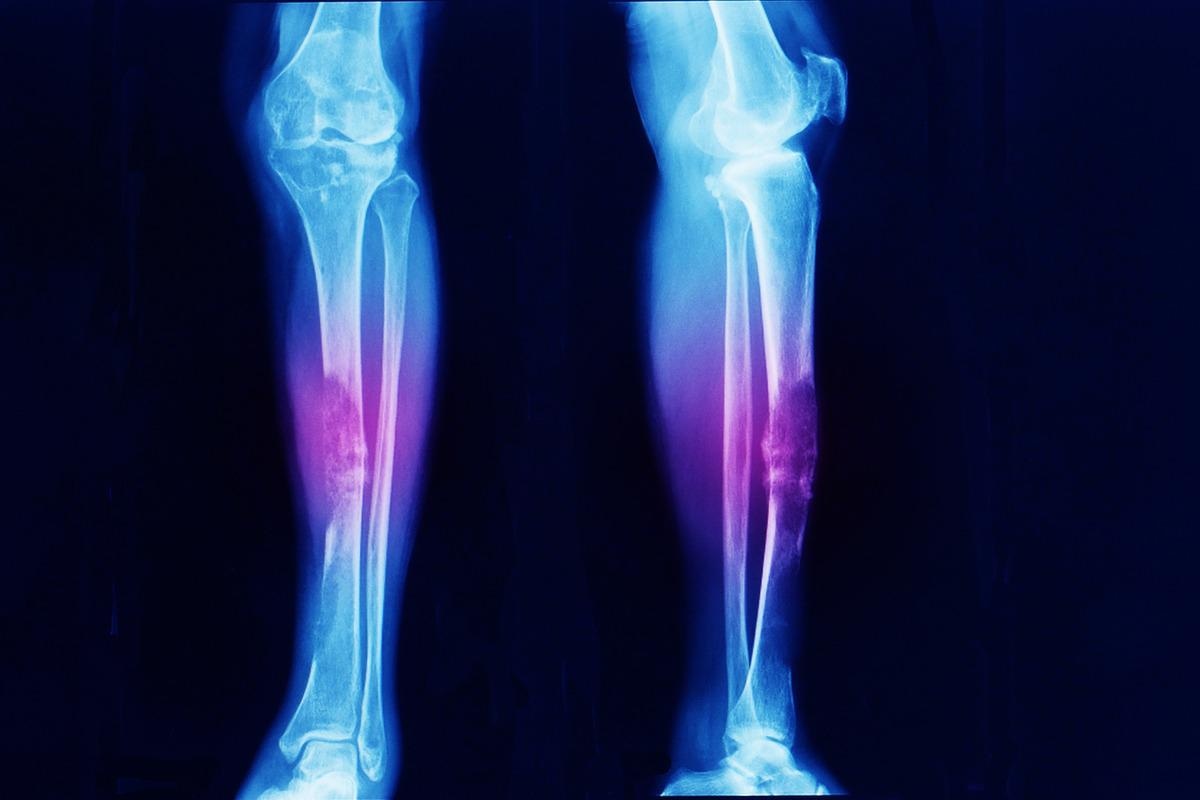 Image Credit: Yok_onepiece/Shutterstock
Image Credit: Yok_onepiece/Shutterstock
Ollier disease and Maffucci syndrome
Multiple enchondromas describe Ollier disease (OD) and Maffucci syndrome (MS). Patients with MS also develop benign vascular overgrowths that, in 8.5 percent of cases, turn malignant. Multiple enchondromas, usually unilateral in distribution and with a preference for the appendicular skeleton, define OD. Multiple enchondromas, which are usually bilaterally distributed, are a hallmark of MS. Multiple swellings on the extremity, deformity around the joints, joint mobility limits, bone shortening, leg-length discrepancy, pain, loss of function, and pathological fractures are all symptoms of both illnesses. OD and MS are rare occurrences. There have been no reports of familial instances yet.
Case reports
Ding et al., in 2019, described a 27-year-old woman who had been hospitalized with paroxysmal headaches and left ptosis for two weeks. A mass was discovered on a magnetic resonance imaging (MRI) scan on the left side of the parasellar area. The lump was surgically removed, and a histopathologic investigation revealed that it was a grade I chondrosarcoma. More imaging tests and a pathologic investigation during follow-up confirmed the ultimate diagnosis of OD.
Wang et al., in 2020, reported a case in which a 37-year-old guy had an evident mass on his left index, middle, and index fingers since the age of six years; nevertheless, no particular treatment was given. The tumors on the patient's hands had grown in size, taking on a dendritic shape, and were accompanied by pain, limiting function and movement after 30 years. Multiple osteopathies of the left hand, left hip, left knee, left ankle, and left foot were discovered on X-ray. A magnetic resonance imaging (MRI) scan of the hip revealed aberrant bone and soft tissue signals in the proximal left femur, raising the possibility of malignant lesions. As a result, the clinical diagnosis of Ollier disease was established.
The 2nd, 3rd, and 4th metacarpophalangeal joints of the left hand were severed and the lesions of the proximal left femur were biopsied after a pre-operative preparation and under brachial plexus anesthesia and local anesthetic. It was advised that a left hip joint dissection be conducted due to the findings that the mass on the left hip joint was malignant; however, the patient and his family could not accept this, and the patient was discharged when his condition was somewhat stable. The patient thought that the function of the left hand was satisfactory after a year and a half of follow-up, but that the lesion on the left thigh had expanded, the local ulcer had ruptured, and the discomfort had become more intense. Three months later, the patient died.
Diagnosis and treatment
Clinical and conventional radiological examinations, rather than genetic testing, are used to diagnose Ollier disease. The most effective method for diagnosing numerous lesions and malignant transformation is radionuclide bone imaging. It can aid in the diagnosis and prognosis of Ollier disease. One of the most basic instruments for diagnosing bone illnesses is an X-ray. The lesions in Ollier disease are mostly oval and develop in the shaft and metaphysis of short or long bones.
The clinical diagnosis of Ollier disease is straightforward, and the majority of patients show no clear sex-related tendency. Ollier disease usually presents as a single or multiple bone mass(es) in the first ten years of life. Ollier disease causes limb abnormalities that worsen with age, affecting children's growth and development.
Surgical removal of the lesions and symptomatic treatment of probable consequences such as pathological fractures, growth defects, and neurological complaints are the only effective treatments. Long-term follow-up is possible for people with Ollier disease who do not have substantial deformities or functional impairment. Bone lengthening surgery can help to repair abnormalities and keep limb development as balanced as feasible. There is presently no specific pharmacological therapy for OD. Amputation may be necessary to lower the risk of recurrence and metastasis after surgery and to improve survival.
References
- Silve, C., & Jüppner, H. (2006). Ollier disease. Orphanet journal of rare diseases, 1, 37. https://doi.org/10.1186/1750-1172-1-37
- Gajavelli, S., Nakhla, J., Nasser, R., Yassari, R., Weidenheim, K. M., & Graber, J. (2016). Ollier disease with anaplastic astrocytoma: A review of the literature and a unique case. Surgical neurology international, 7(Suppl 23), S607–S611. https://doi.org/10.4103/2152-7806.189731
- Ding, C., Chen, W., Liu, F., Xiong, M., & Chen, J. (2019). Skull Base Chondrosarcoma Caused by Ollier Disease: A Case Report and Literature Review. World neurosurgery, 127, 103–108. https://doi.org/10.1016/j.wneu.2019.03.037
- El Abiad, J. M., Robbins, S. M., Cohen, B., Levin, A. S., Valle, D. L., Morris, C. D., & de Macena Sobreira, N. L. (2020). Natural history of Ollier disease and Maffucci syndrome: Patient survey and review of clinical literature. American journal of medical genetics. Part A, 182(5), 1093–1103. https://doi.org/10.1002/ajmg.a.61530
- Wang, J., Li, J., & Wu, Z. (2021). Ollier disease: A case report and literature review. World Academy of Sciences Journal, 3(4), 1-5. https://doi.org/10.3892/wasj.2021.106
Further Reading
Last Updated: Jun 20, 2022