Reactive arthritis (also called “Reiter syndrome”) is a painful inflammatory joint disease. The condition is relatively rare and is more common in men in their twenties and thirties.
Inflammation occurs as a result of bacterial infection of the genitals or colon; however, it may take several weeks for the bacterial infection to transform into reactive arthritis.
Some common pathogens include Chlamydia trachomatis and Neisseria gonorrhea which can cause infection in the genitourinary area; Shigella, Campylobacter, Clostridium, Salmonella, and Yersinia attack the gastrointestinal tract.
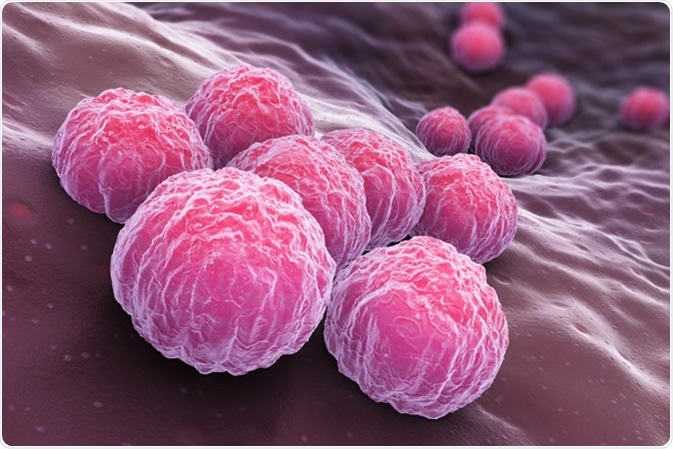
Chlamydia trachomatis, an obligate intracellular human pathogen, is one of four bacterial species in the genus Chlamydia. 3D illustration - Illustration Credit: Tatiana Shepeleva / Shutterstock
The disease is characterized by the classic triad of conjunctivitis, urethritis, and arthritis; however, the triad is not observed in many of the patients.
What causes reactive arthritis?
Autoimmunity is believed to be the primary cause of reactive arthritis. When the causative bacteria reach the blood circulation, T-cells are induced by fragments of bacterial cells, like lipopolysaccharides. The cytotoxic T-cells attack the synovial membrane (the tissue that lines the joints spaces), and this ultimately leads to the characteristic symptoms of the disease.
What are the symptoms of reactive arthritis?
Just as in other forms of arthritis, pain and swelling are the main symptoms of reactive arthritis. The knees, ankles, heels, toes, back and fingers are usually affected. Eye irritation and redness are also found in some patients.
Other common sensations include burning sensation during urination, and skin rashes, especially on the palms and feet. Polyarthritis and cardiac manifestations may occur in the severe form of the disease.
How is reactive arthritis diagnosed?
The diagnosis is made entirely by assessing clinical features; hence it is important to consult a rheumatologist.
The first step is to look for typical symptoms of the bacterial infection, usually occurring from days to weeks after the precipitating infection. Some of these symptoms such as acute oligoarthritis are then correlated with the accompanying musculoskeletal features.
Further investigations may include laboratory tests to confirm the causative bacteria.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) tests are helpful in detecting inflammation. Synovial fluid analysis may also be performed.
Radiographs can be performed to look for inflammation and any joint damage. These can also help to rule out other diseases with similar symptoms.
What are the treatment options for reactive arthritis?
The main goals of treatment include providing symptomatic relief and preventing disease progression. Non-steroidal anti-inflammatory drugs (NSAID) are the drugs of choice in the initial phase.
Glucocorticoids, can be used, either locally or as intra-articular injections, for inflammation. Oral glucocorticoids are generally reserved for severe forms of the disease. Antibiotic therapy is initiated in patients with active infection.
Disease-modifying antirheumatic drugs (DMARDs) are used in patients who do not respond to NSAID therapy. The role of biologics such as tumor necrosis factor (TNF) blocking agents in the treatment of reactive arthritis which is especially severe is also being explored.
Reactive arthritis is a multi-organ disease. Its effective management involves a collaborative effort by a team of rheumatologists, gastroenterologists, ophthalmologists and allied healthcare professionals.
Patient education also plays an important role in improving the quality of life of affected individuals. A healthy lifestyle and regular follow up with specialists can help prevent further complications.
Further Reading
Last Updated: Apr 15, 2019