Skip to
Asthma is an inflammatory condition of the smaller lung airways, which prevents easy breathing. The inflammation is a result of an exaggerated allergic reaction to environmental substances like dust mites, chemicals, dander, mold or pollen. On the other hand, non-allergic asthma is not dependent on allergy, but may be precipitated by other factors like exercise, cold, heartburn, smoke and strong smells.
An asthma attack is characterized by wheezing of varying severity, a tight feeling within the chest caused by the narrowing of the smaller airways, shortness of breath, and coughing. These symptoms are due to tightening of the muscle in the airway walls, and swelling of the mucous lining, besides abnormally increased mucus production. Symptoms differ between individuals, over a wide range of severity. Asthma often first manifests during childhood.

Image Credit: Pathdoc / Shutterstock
Why is asthma sometimes seasonal?
Seasonal asthma is typically allergic asthma. Some common triggers include dust mites, pollen in the air which is also related to hay fever.
Many researchers have recognized that asthma symptoms have a seasonal variation. In many parts of the US, for instance, there are many more cases in early fall, coinciding with the opening of schools, and a second peak often occurs in late fall. Midwinter peaks are well known, and in children below two years of age these are attributed to viral infections like respiratory syncytial virus, or influenza virus. Another smaller peak occurs in spring, with rates then declining irregularly to hit a nadir in summer. Adults, however, tend to show asthma peaks towards the end of the year.
Why are asthma exacerbations in children, also known as asthma attacks, more common during the fall? Scientists think children are have a higher exposure to viral infections and allergens during this season as schools also reopen around this time. However, rhinoviruses and other viral pathogens are known to provoke flare-ups throughout the year, rather than only in fall or spring.
Seasonal allergies
People with asthma who also have allergies are at a significantly higher risk of asthma exacerbations. The presence of allergic inflammation is associated with high levels of immunoglobulin E (IgE), an antibody specifically linked to allergic phenomena. When this antibody is present at high levels, as in allergic states, viral infection is much more likely to result in serious asthma attacks.
Some pertinent studies show that patients who are exposed to more dust mites and pollen in the autumn, which can cause allergic reactions in susceptible people, experience more flare-ups at this time. Similarly, more attacks occur during hay fever season (spring and early summer) in asthma patients who are sensitive to grass. Seasonal asthma is thus linked to allergen exposures at various periods of the year.
An understanding of this process will potentially help the development of preventive measures. In fact, one study used an anti-IgE monoclonal antibody to dramatically reduce seasonal asthma peaks in children living in an inner-city region, supporting the theory that allergen exposure contributes to asthma symptoms.
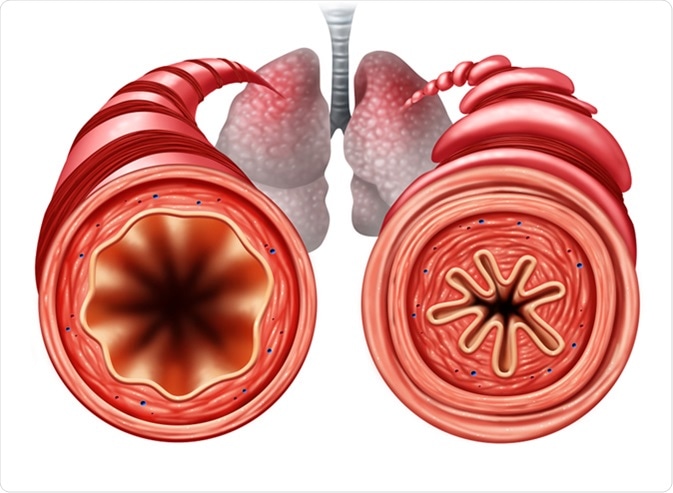
Asthma diagram as a healthy and unhealthy bronchial tube with a constricted breathing problem caused by respiratory muscle tightening. Image Credit: Lightspring / Shutterstock
Seasonal climate variations
Climate variation in different geographical regions also plays a role in seasonal asthma exacerbations. In cold weather children spend more time indoors and are therefore exposed to increased levels of pests, mold and dust mites. In summer, despite the heat and humidity, the absolute exposure to such allergens is likely to be lower and this may account for the widespread drop in asthma during this season.
Similarly, ‘thunderstorm asthma’, which occurs once in about five years in some locations, may be due to the rapid increase in grass and mold allergens coupled with high rainfall and humidity at this time, which affects susceptible people.
Combined factors
People with asthma who are sensitized to grass, birch pollen and a type of fungi called Alternaria experience modified seasonal patterns. Grass sensitivity is linked to increased asthma attacks during summer in this population, when other asthma patients typically have the lowest number of attacks. Similarly, birch pollen exposure peaks in May-August in northern Europe, but the peak is much shorter and more intense in the south of the continent. It is thought that the antigenic nature of the pollen may be more important than the absolute amount of pollen in the air.
Other factors
The pattern of seasonal asthma is also modified by air pollution and tobacco smoke. An algorithm that accounts for all these risk factors may help predict asthma flare-ups in children on a seasonal basis, but requires more real-time observation of environmental and climatic factors in association with actual patients.
For optimal application, asthma control measures must consider the time of year, local environment and geographic region, along with individual-specific risk factors. This will help doctors recommend appropriate preventive and treatment measures at peak times for children with asthma. More research is needed to understand how environmental exposures correlate with seasonal asthma peaks to help predict and prevent serious asthma attacks at certain seasons.
Sources
- Nhlbi.nih.gov. Asthma. https://www.nhlbi.nih.gov/health-topics/asthma
- Cohen H. A., et al., (2014). Seasonality of Asthma: A Retrospective Population Study. Pediatrics. https://pediatrics.aappublications.org/content/133/4/e923
- Wiesniewski J. A., et al., (2016). A comparison of seasonal trends in asthma exacerbations among children from geographic regions with different climates. Allergy and Asthma Proceedings. https://dx.doi.org/10.2500%2Faap.2016.37.3994
- De Verdier G., et al., (2017). Seasonal and geographic variations in the incidence of asthma exacerbations in the United States. Journal of Asthma. doi: 10.1080/02770903.2016.1277538, https://www.ncbi.nlm.nih.gov/pubmed/28102717
- Pike K. C., et al., (2018). Interventions for autumn exacerbations of asthma in children. doi: 10.1002/14651858.CD012393.pub2. https://www.ncbi.nlm.nih.gov/pubmed/29518252
- Canova C., et al., (2013). The influence of sensitisation to pollens and moulds on seasonal variations in asthma attacks. European Respiratory Journal. DOI: 10.1183/09031936.00097412, https://erj.ersjournals.com/content/42/4/935
- Silver J. D., et al., (2018). Seasonal asthma in Melbourne, Australia, and some observations on the occurrence of thunderstorm asthma and its predictability. PLOS One. https://doi.org/10.1371/journal.pone.0194929
Further Reading
Last Updated: Aug 19, 2019