Sézary syndrome represents a type of blood malignancy belonging to the group of T-cell lymphomas which are known to affect the skin.
Skip to
This syndrome is characterized by widespread skin lesions and swollen lymph nodes; however, the malignant T-cells can spread and affect organs such as lymph nodes, liver, bone marrow and spleen. The malignant cells are also known as Sézary cells, they harbour a characteristic cerebriform nucleus, and are found in the blood, skin, and lymph nodes.
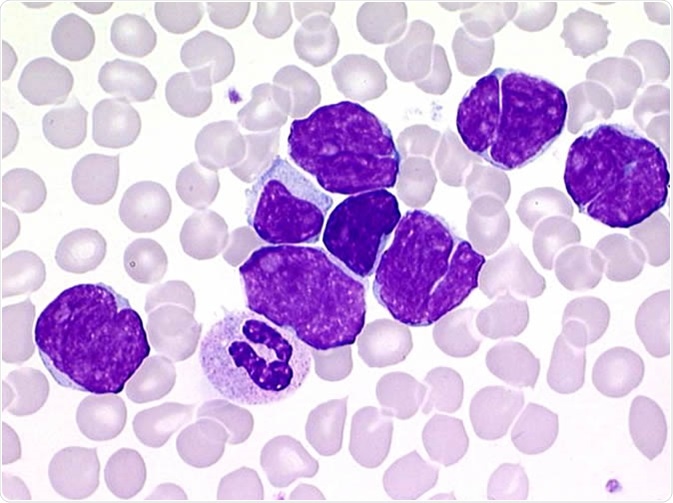
Sézary cells
Sézary syndrome leads to suppression of the immune system, hence the affected patients are at a high risk of developing secondary infections. They also have a high propensity to develop other types of lymphoma - most notably Hodgkin and non-Hodgkin lymphomas.
The syndrome is commonly found in people aged 60 and above and is associated with a very low survival rate. Sézary syndrome is predominantly found in males and is more common in individuals with an African-Americans descent. In addition, some rare cases of Sézary syndrome have been found in children too.
Sézary syndrome is closely related to mycosis fungoides, which is yet another form of T-cell lymphoma pertinent to skin. Mycosis fungoides is characterized by the presence of a patch or a plaque, whereas Sézary syndrome is identified by the presence of a widespread skin rash.
What are the causes of Sézary syndrome?
The exact etiology of Sézary syndrome is not known. Certain chromosomal (particularly chromosomes 8, 10 and 17) abnormalities have been observed in the majority of the patients, which is in line with other malignancies as well. The disease is seen sporadically in individuals without family history of the condition.
Infectious events in mycosis fungoides/Sézary syndrome, R. Blaizot et al
What are the signs and symptoms of Sézary syndrome?
Skin lesions and enlarged lymph nodes are the two commonly associated symptoms with this condition. Fever, edemas, alopecia, thick and hard skin, nails abnormalities and ectropion (a condition in which the lower eyelid turns outwards) are some other symptoms of Sézary syndrome. It has been observed that some patients with Sézary syndrome are not able to maintain their body temperature.
How is Sézary syndrome diagnosed?
Assessment of the characteristic symptoms is the initial step in diagnosis. Laboratory test to assess a complete blood count is initially performed. Peripheral blood smear, immunophenotyping, T-cell receptor (TCR) gene rearrangement test and flow cytometry can also aid in the diagnosis.
Enlarged lymph nodes can be identified by using computed tomography (CT) scan and positron emission tomography (PET) scan. The chest, abdomen and pelvis are usually examined. A skin biopsy can be done to confirm the diagnosis.
Staging for cutaneous Sézary syndrome is based on an evaluation of the skin, lymph nodes, viscera, and blood. The stages range from I to IV, in accordance with the severity of the condition.
What are the treatment options for Sézary syndrome?
Treatment for Sézary syndrome is decided after assessing the symptoms and the severity of the illness. Naturally, the main focus of any therapy is to destroy the malignant T-cells and correct the immune imbalances caused by the malignant lymphocytes.
Phototherapy can be used to treat skin lesions; likewise, radiation therapy and chemotherapy can be used to destroy cancerous cells. Steroids can be effective in controlling the itchy skin.
Biologic therapy and targeted therapy represent novel therapy options which have fewer side-effects compared to the conventional therapies. Stem cell transplantation can be used in younger patients with severe disease.
Diagnostic and therapeutic considerations
Sézary syndrome has certain dermatological features which are often confused with other skin diseases such as atopic dermatitis. A better understanding of the disease pathophysiology and the identification of potential biomarkers can lead to certain improvements in the treatment of Sézary syndrome.
Several novel diagnostic markers and treatment options have been discovered; however, there is still a dire need for efficacious therapy. Blocking the immune pathways which are controlled by the malignant T cells can be beneficial in treating this condition. Techniques and therapies aimed at improving the survival rate and the quality of life of the affected individuals are warranted.
Further Reading
Last Updated: May 17, 2019