Bursitis is a condition in which the joints become tender and painful. It occurs when bursae, small sacs filled with fluid that cushion the joints, become inflamed. Studies have found that non-operative treatment methods are most effective in treating the condition. It is thought to affect around 5.6 patients per 1,000 adults.
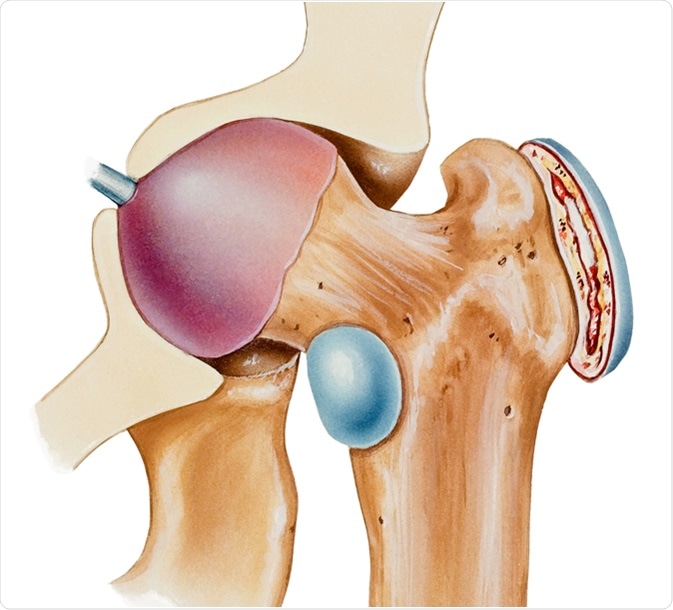
Hip - Bursitis. A bursa is a fluid filled sac that facilitates the smooth motion of joints. Image Credit: Medical Art Inc / Shutterstock
Where are Bursae Found?
Bursae are located in the shoulder, elbow, hips, knees, and heels. They are found between the bones and soft tissues of these joints, and exist to reduce friction in the area.
Why does Trochanteric Bursitis Occur?
Bursitis occurs when the bursa’s outer lining, called the synovial membrane, becomes inflamed.
Trochanteric bursitis describes bursitis of two particular bursae in the hip. One bursa is found on the greater trochanter, and the other is found in the groin-side of the hip, and is called the iliopsoas bursa. Inflammation of the iliopsoas bursa on the inside of the hip is less common than inflammation of the bursa covering the greater trochanter, which takes the name trochanteric bursitis.
What are the symptoms of Trochanteric Bursitis?
Trochanteric bursitis presents the following symptoms:
- Pain on the lateral (outside) point of the hip.
- Pain in the thigh or buttock
- Pain when lying on the affected hip
- Pain when pressure is applied to the hip
- Pain after getting out of chairs or a car
- Pain while climbing stairs.
Risk factors for Trochanteric Bursitis
A number of risk factors have been identified in the development of trochanteric bursitis. These include:
Repetitive stress injury
Frequently running, climbing stairs, standing for extended periods of time, or cycling can contribute to developing trochanteric bursitis.
Injury to the hip
A fall onto the point of the hip can result in injury, causing traumatic bursitis. Sometimes, the bursa can fill with blood and, although the blood is eventually reabsorbed, the bursa lining can remain inflamed. Lying on one side of the body for an extended period of time can also result in trochanteric bursitis.
Diseases of the spine
Several spinal diseases including scoliosis and lumbar arthritis (arthritis of the lower spine), among others, can contribute to trochanteric bursitis.
Unequal leg length
Walking differently to compensate for inequality in leg length can result in hip bursa irritation.
Rheumatoid arthritis and gout
Rheumatoid arthritis increases the risk of bursae becoming irritated as the condition affects the synovial membranes found in joints. Gout develops when there is an accumulation of urate crystals in synovial joints, leading to irritation.
Previous surgeries
Surgeries around the hip or the use of prosthetic hip implants can cause bursae to become inflamed.
Bone spurs or calcium deposits
The bursae can become irritated when bone spurs or calcium deposits form within tendons that attach muscles to the trochanter.
Age and gender
Women are more likely to develop hip bursitis. It is more often seen in people over 40, but people of any age can be affected.
Diagnosis of Trochanteric Bursitis
A physical examination is required to diagnose trochanteric bursitis. This is to determine any points of pain or tenderness, and to identify any swelling.
In some cases, an X-ray or magnetic resonance imaging (MRI) scan can be used if fractures or osteoarthritis is causing the hip pain. Any abnormalities or damage to the bursae or tendons will be able to be identified with an MRI scan.
In rarer cases, the bursa can become infected by bacteria, and septic hip bursitis results. In these cases, a doctor will perform a procedure called aspiration, in which the fluid from the bursa is removed with a needle and syringe.
The fluid taken from this procedure can be evaluated for the presence of bacteria, white blood cells, and glucose level to determine whether or not infection is present.
Treatment of Trochanteric Bursitis
Modifying the amount or intensity of activities can ease symptoms of trochanteric bursitis. Physical therapy, weight loss, corticosteroid injections, aspiration, antibiotics (in the case of septic hip bursitis) and non-steroidal anti-inflammatory medications (NSAIDs) are also effective treatments.
However, recurrence of bursitis is common, and patients often have to undergo further treatment to remedy the pain caused by trochanteric bursitis.
Rarely, surgery is needed to correct trochanteric bursitis. The following surgical procedures can be warranted in these cases:
Bursectomy
An incision is made at the hip and the bursa is removed. Arthroscopic (keyhole) bursectomies can be carried out to reduce healing time and the risk of complications.
Iliotibial band release
When the root cause of hip bursitis is problems with the iliotibial band or other tendons, tendons can be repaired and reattached to the greater trochanter. Iliotibial band release involves lengthening the band to reduce friction and therefore inflammation and irritation. A bursectomy may be carried out at the same time as these procedures.
Osteotomy of the greater trochanter
In this procedure, a surgeon will shave off a small amount of the greater trochanter bone, which can reduce friction and associated pain.
Summary
Although trochanteric bursitis normally affects people over the age of 40, it can affect people of any age, and women are more likely to develop hip bursitis than men. Most treatments for the condition include home treatments such as physical therapy, rest, and activity modification, however injections and surgeries are available to correct the problem. Surgery is rarely needed, but several non-surgical treatments may be needed to alleviate pain caused by trochanteric bursitis.
Further Reading
Last Updated: Apr 3, 2019