Introduction
What causes urethritis?
Urethritis symptoms and complications
How is urethritis diagnosed?
How is urethritis treated?
Prevention
References
Further reading
Introduction
Urethritis is a medical condition that involves inflammation of the urethra, the tube through which urine is removed from the bladder. Urethritis is characterized by swelling and irritation in the urethra, often accompanied by pain during urination (dysuria) and sexual intercourse (dyspareunia), penile discharge, and pelvic pain.
 Image Credit: Albina Gavrilovic / Shutterstock
Image Credit: Albina Gavrilovic / Shutterstock
What causes urethritis?
It most often occurs as a result of an infection by bacteria or viruses. Sexually transmitted diseases like chlamydia and gonorrhea are the predominant cause of urethritis. However, other bacteria and viruses such as Escherichia coli, herpes simplex virus, and cytomegalovirus may all be responsible for the infection.
Urethritis can be classified into two types according to the cause. Gonococcal urethritis is a result of an infection by the bacterium Neisseria gonorrhoeae. Nongonococcal urethritis (NGU) is urethritis caused by agents other than gonorrhea. Causal agents of NGU could include various other sexually transmitted infections or diseases (STI/STD), injury to the area, and chemicals used in the pelvic region, such as spermicides, contraceptive jellies and creams, deodorant tampons, douches, and irritant personal lubricants.
 Bacteria Neisseria gonorrhoeae. Image Credit: Giovanni Cancemi / Shutterstock
Bacteria Neisseria gonorrhoeae. Image Credit: Giovanni Cancemi / Shutterstock
Some of the etiological vectors of NGU are Chlamydia trachomatis, Ureaplasma urealyticum, Trichomonas vaginalis, Mycoplasma genitalium, the Herpes simplex virus, cytomegalovirus, and the sore throat causing adenovirus. Injury to the urethra during vigorous masturbation or sex or damage to the urethra during a medical procedure, such as inserting a urinary catheter, can also cause NGU. Nongonococcal urethritis is also sometimes called non-specific urethritis (NSU).
As sexually transmitted diseases can cause urethritis, people who have unprotected sex and with multiple partners usually have a higher risk of contracting the infection.
Urethritis symptoms and complications
Due to differences in the anatomy of the urethra between males and females, the symptoms experienced by those affected by the condition often differ considerably.
Many women do not notice any symptoms, although they may experience abdominal pain and a burning sensation during urination. Other symptoms experienced by women include frequent urination, vaginal discharge, and fever.
Men more commonly report symptoms such as:
- Presence of blood in urine and/or semen
- Dysuria
- White discharge from the penis
- Frequent urination
- Inflamed penis, including itching and swelling
- Lymph node enlargement
- Pain on ejaculation
The penile discharge in gonococcal urethritis is often green, yellow, or white and contains pus. Nongonococcal urethritis discharge is often white or clear.
Timely diagnosis and treatment of urethritis almost certainly clear up the symptoms. However, a severe infection that is not treated adequately may lead to further complications, such as an infection of the bladder, the testicles, or the cervix, depending on the gender of the individual.
Untreated gonococcal urethritis can lead to systemic infections, tenosynovitis, and reactive arthritis. If the infection spreads through the bloodstream, it could also cause endocarditis and meningitis. In addition, if left untreated, NGU can cause pelvic inflammatory disease (PID) in women, which manifests as severe pain near the pelvis and lower abdomen, discomfort in the pelvic region during and bleeding after sexual intercourse, high temperature, and green or yellow vaginal discharge. Women are also at risk of bladder infections and cervicitis if urethritis is left untreated. It may also get transmitted to infants from infected mothers, resulting in middle ear infections, conjunctivitis, or even pneumonia.
Both types of urethritis can cause abscesses in the tissue surrounding the urethra and lead to urethral fibrosis and stricture. Other complications include epididymitis — infection of the epididymis, testicular atrophy and infertility, and prostatitis.
How is urethritis diagnosed?
The initial diagnosis usually involves a physical examination of the urethra to detect signs of redness, discharge, and swollen lymph nodes.
A swab and a urine test are taken to diagnose both types of urethritis. A swab is then taken from inside the urethra, which can be a painful procedure for the patient as no lubricant is used, and is examined in a laboratory for evidence of infection. A urine leukocyte esterase test to detect the presence of white blood cells is also sometimes used to detect or confirm urethritis. In the absence of urethral discharge, the first-void urine is tested for the presence of pus, and DNA-based tests for gonorrhea and chlamydia are ordered.
Tests for other STIs are recommended to reliably diagnose and treat the disease. Testing for urethral pathogens other than N. gonorrhoeae and C. trachomatis is prescribed only in cases with persistent and unexplained symptoms.
If it is a male patient, a digital rectal exam may be needed to test the prostate gland for any associated swelling or inflammation that could be causing symptoms. Palpation of the scrotum for signs of epididymitis is also carried out in some cases.
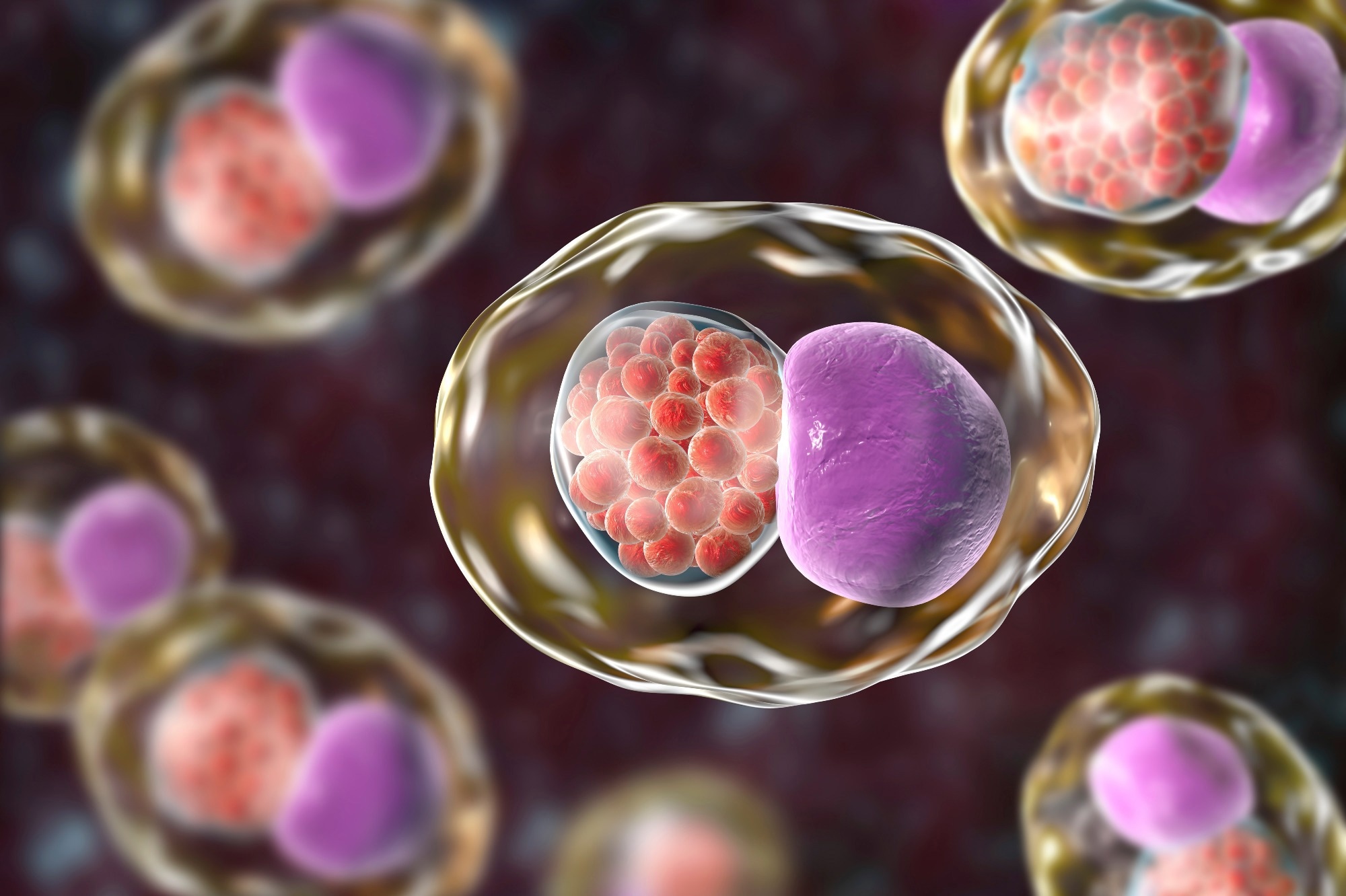 Chlamydia trachomatis bacteria, 3D illustration showing reticulate bodies of Chlamydia forming intracellular intracytoplasmic inclusions (small red) near the cell nucleus (purple). Image Credit: Kateryna Kon / Shutterstock
Chlamydia trachomatis bacteria, 3D illustration showing reticulate bodies of Chlamydia forming intracellular intracytoplasmic inclusions (small red) near the cell nucleus (purple). Image Credit: Kateryna Kon / Shutterstock
How is urethritis treated?
The primary aim of treatment is to eradicate the infection, which will help improve symptoms and prevent the spread of infection. Abstinence is strongly recommended during treatment, including oral and anal sex abstinence. Additionally, any regular sexual partner should also be treated, regardless of whether or not they have symptoms, as they may also carry the pathogen. The specific treatment for each individual depends on the cause of the infection.
Gonococcal urethritis is usually treated with a 125 mg intramuscular dose of ceftriaxone or 400 mg oral cefixime. Alternate treatments for gonococcal urethritis include ciprofloxacin, ofloxacin, and spectinomycin, although fluoroquinolone treatments for gonorrhea are being gradually discontinued due to increased resistance. Treatment with 100 or 200 mg doses of doxycycline is recommended to treat coexisting chlamydia infections.
Standard treatments for NGU include oral azithromycin or doxycycline for a week. Alternate therapies include erythromycin, levofloxacin, clotrimazole, fluconazole, metronidazole, and trimethoprim, used either alone or in combination. In cases of accompanying trichomoniasis, metronidazole or tinidazole is also prescribed.
Common side effects of the antibiotic treatment include diarrhea, nausea, gastrointestinal upset, dyspepsia, hypersensitivity reactions, and in some cases, photosensitivity. Doxycycline is known to cause hepatic toxicity.
If bacterial and viral causes have been ruled out, and a chemical irritant is more likely to be the cause, discontinuing the use of the product with the irritant, and waiting for symptoms to subside is the best course of action. Patients are advised to use fragrance-free soaps and lubricants, increase hydration, discontinue the use of spermicides, and reduce penile trauma by practicing infrequent and less vigorous intercourse and masturbation.
Pain relief medication such as acetaminophen, ibuprofen, and phenazopyridine may also be indicated to provide an immediate analgesic effect before the antibiotics begin to take action.
Once the infection has improved and symptoms have subsided, future infections may be prevented with several precautionary methods. It is essential to maintain cleanliness standards, particularly around the opening of the urethra. Additionally, it is best if any sexual activity is adequately protected with the use of condoms, which is even more important if there are multiple partners with unknown sexual histories. Finally, notifying and treating the patient’s sexual partners is vital to preventing persistent and recurring infections.
How Is Urethritis Treated?
Prevention
Safe sex is the primary method to prevent urethritis. Using barrier contraceptives such as condoms and water-based lubricants, limiting the number of sexual partners, and getting frequently tested for STIs and STDs in case of multiple sexual partners contribute to preventing urethritis and associated infections. Avoid chemicals and excessive physical force that could damage the urethra. Practicing good personal hygiene also prevents urethritis and other urinary tract infections. An intact urethral endothelium is an important barrier to the spread of many bloodborne infections, including the human immunodeficiency virus (HIV).
References
Further Reading
Last Updated: Sep 6, 2022