The human heart is a powerful muscular organ which has the responsibility of directing blood in two parallel and vital circulations.
 Credit: Katryna Kon/Shutterstock.com
Credit: Katryna Kon/Shutterstock.com
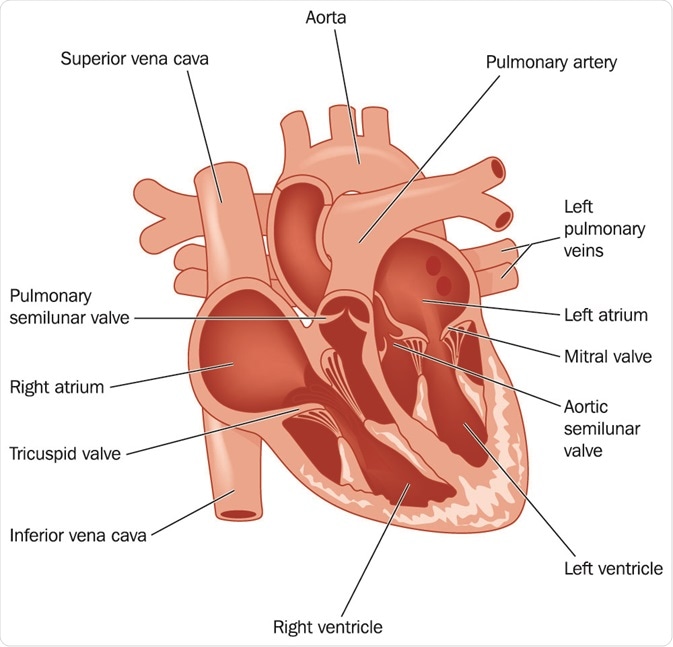
It is divided into two upper and two lower chambers, termed the atria and the ventricles, respectively. The left atrium and left ventricle form one system which receives blood (which has been oxygenated) from the lungs and pumps it to the whole body from the ventricle. These two chambers are separated by the mitral valve, and the ventricle is separated from the aorta, the great vessel through which blood reaches the rest of the body, by the aortic valve.
On the right side, the right atrium and ventricle receive (deoxygenated) blood from the body and pump it to the lungs for oxygenation and purification. This is then returned to the left side of the heart. The right chambers are separated by the tricuspid valve, and the right ventricle is separated from the large pulmonary trunk (which takes blood to the lungs) by the pulmonary valve.
The function of these valves is to keep blood flowing in only one direction, so that bodily functions can proceed smoothly with the uninterrupted supply of oxygen-rich blood. They are composed of fibrous tissue overlaid by an exquisitely smooth and slippery layer called the endocardium, which ensures that the blood flows over and through them with minimum friction. This reduces wear and tear on the heart and also keeps the blood in the fluid form, instead of clotting.
The valves are connected to the heart muscle through a tough valve ring or annulus, and the leaflets of the mitral and tricuspid valves are held to the heart muscle by thin tough cords called the chordae tendinae.
Types of valve damage or abnormality
Trauma, infection, degeneration, cardiovascular disease, or congenital anomalies, may all affect the structure and functioning of these valves. This may lead to dysfunctions such as:
- Stenosis when the heart valve is too narrow for proper blood flow: this reduces the blood flow to the distal chamber or vessel and results in strain on the pumping chamber, causing it to thicken and making it prone to anginal pains caused by the insufficiency of oxygen supply to the heart muscle
- Regurgitation when the blood leaks backward from one chamber to the previous one: this causes blood to pool in the first chamber, distending and weakening it, and also deprives the pumping chamber of enough blood to deliver to the next location
- Atresia when a heart valve fails to develop at all
Eventually, severe valve disease results in heart failure and thrombotic complications in many cases.
Common heart valve diseases:
- Congenital anomalies: bicuspid aortic valve, Ebstein’s anomaly (of the pulmonary valve)
- Degenerative or age-related valve disease: mitral valve prolapse, aortic stenosis, post-irradiation valvular disease
- Rheumatic heart disease: autoimmune damage to any of the valves, most commonly the mitral valve
- Infective endocarditis: bacterial infection leading to damage to the heart valve tissue
- Trauma to the chest
 Credit: Blamb/Shutterstock.com
Credit: Blamb/Shutterstock.com
Clinical features
Most people may feel symptoms such as dyspnea (shortness of breath), cough with sputum, swelling of the feet or ankles, or palpitations when the heart valves are severely affected. Serious complications include heart failure, cardiogenic shock, infective endocarditis sudden death.
Diagnosis
The primary sign of valve disease is a heart murmur, an abnormal sound heart while listening to the heart beat sound with a stethoscope. Different types of valve abnormalities have different murmurs which may range from a blowing to a clicking sound at various times. The diagnosis is confirmed by echocardiography, which produces a detailed picture of the heart and its valves, with Doppler echocardiography to study blood flow.
Other studies which may be required include coronary angiography, ECG, and MRI of the heart.
Treatment
Treatment of heart disease is both medical and surgical. Medications are required, especially in the early stages, to improve heart function and ease pain. These may include digitalis, diuretics to expel excessive retained fluid from the body, antiplatelet and/or anticoagulant drugs to lower the risk of blood clots in the heart chambers. Calcium channel blockers and beta-adrenergic blockers are needed to reduce the workload of the heart.
However, functional restoration is possible only through surgical intervention. Lifestyle changes help ensure that no unnecessary load is placed on the heart, thus relieving its strain, and preventing further damage from infections such as infective endocarditis and rheumatic fever. Antibiotic prophylaxis is often needed before certain surgical procedures to avoid such infections.
Both open and percutaneous surgery is carried out for valve repair and replacement. Balloon valvuloplasty is one such procedure which opens narrowed valves using an inflatable balloon to stretch the damaged rigid tissue and so enlarge the opening. Valves may be replaced if severely damaged, by biological or mechanical valves. The latter have a longer lifetime, but the patient must be on anticoagulant drugs lifelong to prevent blood clots from forming on the artificial valve surfaces. Minimally invasive procedures have also been developed for patients who are not fit for open surgery.
Further Reading
Last Updated: Dec 29, 2022