VLP stands for virus-like particles. Virus-like particles are molecules that mimic viruses but are not infectious. They are a very effective way of creating vaccines against diseases such as human papillomavirus (HPV), hepatitis B, malaria, and more.
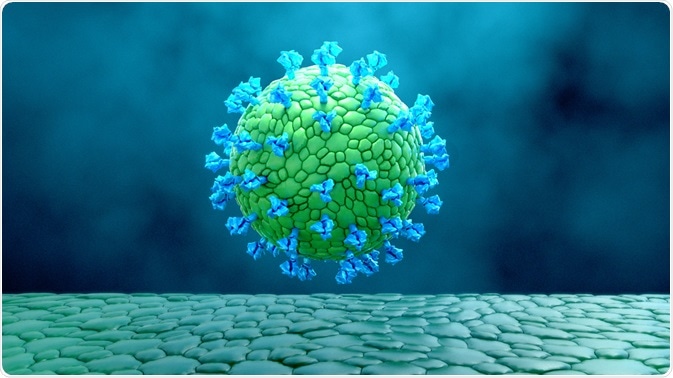
Image Credit: Design_Cells/Shutterstock.com
How do VLP vaccines work?
A virus-like particle is not infectious because it does not contain any viral genetic material. As they are very similar to real viral molecules, introducing a VLP into the body will trigger an immune response, but a person will not experience any symptoms of the virus they are being vaccinated against.
Once the body has had an immune response to the VLP, it will recognize the virus and prevent infection in the future, giving people immunity to that particular virus.
A VLP consists of one or more structural proteins that can be arranged in multiple layers. They can also contain an outer lipid envelope, which is the outermost layer that covers a large number of different viruses. This outer layer protects the genetic material inside the virus particle. In some viruses, envelopes can contain material from the person that has been infected with the virus, which helps them to go undetected by the immune system.
Creating a VLP vaccine can use bacterial, yeast, insect, or mammalian cells. The type of cell that is chosen depends on how much it will cost to produce a vaccine in this way, and whether the VLP will need to be later modified to trigger the strongest immune response possible through post-translational modifications (PTMs).
One study concluded that in 174 VLPs, bacterial systems were used in 28% of cases to make the VLP, yeast systems were used in 20%, and insect systems were used in 28%. Plant and mammalian systems were used in 9% and 15% of cases respectively.
Types of VLP vaccines
There are many different types of vaccine, including:
VLP vaccines are a type of recombinant vaccine, but they offer the efficiency of a live-attenuated vaccine. Recombinant vaccines use a particular piece of the germ that the immune system targets specifically.
Typically, the immune response to this type of vaccine is very strong, but it is sometimes necessary to top up the vaccine overtime to maintain immunity. One key advantage of a recombinant vaccine is that it is suitable for use in people with weakened immune systems.
There have been around 110 VLPs made from viruses belonging to 35 different families, with interest in this area growing substantially.
The human papillomavirus vaccine (also called a cervical cancer vaccine), which is first offered to girls and boys between the age of 12 and 13, is one type of commonly used VLP vaccine. In the HPV vaccine, the VLPs are formed by the main capsid protein, L1, which is the protein found on the casing of the germ.
Virus-like particles are also very small, with a particle radius of approximately 20 to 200 nm. This means that they can easily enter the lymph nodes, where the immune system is activated in the case of an infection, and VLPs have been shown to reach the lymph nodes in under 10 minutes.
Also due to their small size, VLPs can be taken on by antigen-presenting cells (APCs), which present disease particles to lymphocytes so that the immune system will recognize them in the case of an infection. Once taken on by an APC, VLPs can be degraded and activate a T-cell response. T cells are part of the body’s immune response to infection.
There are growing numbers of studies that discuss the development of vaccines that are made based on nanoparticles, which include VLPs. The advantages of these nanoparticle-based vaccines are that they are believed to possess high specificity, are very efficient, and have good pharmacokinetic characteristics.
Nanoparticle-based VLP vaccines may also eliminate the need for vaccines to be injected, and could potentially be given in intranasal vaccines or inhalers.
 Image Credit: New Africa/Shutterstock.com
Image Credit: New Africa/Shutterstock.com
What are the benefits of a VLP vaccine?
VLP vaccines benefit from the VLP’s ability to present antigens in a repetitive manner, which allows for the cross-linking of B cell receptors (BCRs).
VLPs have repetitive surface patterns and a particulate structure that triggers strong immune responses, which helps a person build up good immunity to a disease. They have also been shown to be very safe, both for the person being vaccinated and for the people producing and administering the vaccines.
This is because there is no viable viral material in the virus-like particle, meaning that the people producing the vaccine could not contract the virus themselves. This also means that anyone administering the vaccine will not contract the virus if they are exposed to the particles.
As viruses are prone to mutate, making previous vaccines ineffective in some cases, VLPs are a promising option to combat this issue. This is because the surface proteins of a VLP can be modeled to fight against a specific combination of proteins on a novel version of a virus.
VLPs are also not able to replicate, which makes them safer than attenuated vaccines in some respects.
What are the risks of a VLP vaccine?
The risks of VLP vaccines are largely the same as other types of vaccines. Any side effects experienced will likely depend on the disease a person is being vaccinated against.
Common side effects of vaccination include:
- Pain, swelling, or redness where the vaccine was injected
- Mild fever
- Chills
- Fatigue
- Headaches
- Muscle aches
- Joint aches
These side effects are a sign that the immune system is building up a response to protect the body from the disease being vaccinated against.
If the vaccine is injected, there is a small risk of infection at the injection site, as any break in the skin can carry a risk of infection.
Overall, being vaccinated against the disease is safer than contracting the disease itself.
Summary
Using virus-like particles to develop vaccinations against infectious viral diseases is becoming an increasingly popular area of study since the success of the HPV vaccine. VLP vaccines are being used more and more often due to their increased safety and ability to trigger strong immune responses, and their ability to be made on a large scale and their potential for being used in inhaled vaccinations over injected vaccinations is an attractive advantage over other types of vaccine.
There have been several VLP vaccines widely accepted onto the market, such as the HPV and hepatitis B vaccine, and there has been some success with a VLP malaria vaccine, with many more types of VLP vaccine targeting other diseases currently being developed.
References
- Akahata, W. et al. Development of a novel virus-like particle vaccine platform that mimics the immature form of alphavirus. (2017). https://cvi.asm.org/content/24/7/e00090-17
- Anderson, D. A., Grgacic, E. V. L. Virus-like particles: passport to immune recognition. (2006). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7128828/
- Bachmann, M. F. et al. Interaction of viral capsid-derived virus-like particles (VLPs) with the innate immune system. (2018). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6161069/
- Cervera, L. et al. Production of virus-like particles for vaccines. (2017). https://www.sciencedirect.com/science/article/abs/pii/S1871678416325511
- Garg, H. et al. Virus-like particles (VLP) as multivalent vaccine candidate against Chikungunya, Japanese encephalitis, yellow fever, and Zika virus. (2020). https://www.nature.com/articles/s41598-020-61103-1
- Ilyin, Y. V., Syomin, B. V. Virus-like particles as an instrument of vaccine production. (2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7088979/
- Noad, R., Roy, P. Virus-like particles as a vaccine delivery system: myths and facts. (2008). https://www.tandfonline.com/doi/pdf/10.4161/hv.4.1.5559
- Vaccines. Vaccine side effects. (2020). https://www.vaccines.gov/basics/safety/side_effects
- Vaccines. Vaccine types. (2020). https://www.vaccines.gov/basics/types
- Zeltins, A. Construction and characterization of virus-like particles: a review. (2012). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7090963/
Last Updated: Mar 17, 2021