Parkinson’s disease is a progressive neurodegenerative disorder characterized by a loss of dopaminergic neurons in a specific brain region called substantia nigra, which is typically involved in the regulation of reward and movement. Although a brain disorder, a growing pool of evidence suggests that Parkinson’s disease may originate in the gut.

Image Credit: Kotcha K/Shutterstock.com
What is Parkinson’s disease?
Parkinson’s disease is the 2nd most common age-related neurological disorder worldwide, affecting about 3% of people aged 65 or more and 5% of people aged over 85.
Although the exact etiology is unknown, the primary cause of Parkinson’s disease is believed to be an abnormal accumulation of a protein called alpha-synuclein (Lewy bodies) in dopaminergic neurons, leading to impairment in neuronal activity.
The reduction in dopamine levels in the brain causes abnormal brain activities, which are mainly associated with tremor, muscle stiffness, movement difficulty, and balance problems.
Besides motor- or movement-related symptoms, Parkinson’s disease can be associated with cognitive deficits, depression, apathy, loss of smell sensation, chewing and swallowing difficulty, sleep disorders, constipation, urination-related difficulties, orthostatic hypotension, and fatigue.
Does Parkinson’s disease originate in the gut?
The idea
In 1817, James Parkinson, an English surgeon, for the first time proposed the connection between Parkinson’s disease and the gut.
He reported that the treatment of constipation-related problems caused improvement of motor symptoms in one out of six patients with Parkinson’s disease.
Since then, many studies focusing on the etiology of Parkinson’s disease have found that constipation is one of the key symptoms of the disease, and it often appears just before the onset of motor-related problems.
The innovation
In 2003, the breakthrough in this particular field came with the observation that instead of the brain, Parkinson’s disease may be developed in the gut.
A study conducted by the neuroanatomist, Heiko Braak, has found that apart from specific brain neurons, Lewy bodies are present in parts of the central nervous system that controls the gastrointestinal tract.
Also, the study findings have hypothesized that the pathological alterations in the gut can eventually translocate to the central nervous system by a ‘yet unidentified pathogen’ that crosses the mucosal barrier of the gastrointestinal tract and travels via the vagus nerve to reach the brainstem.
Proof of concept
Recently, a study has been conducted to prove the hypothesis of Heiko Braak and colleagues. The experiment has been conducted by injecting synthetic misfolded alpha-synuclein in the gut of healthy mice and collecting the brain tissue samples after 1, 3, 7, and 10 months of injection.
The findings have revealed that misfolded proteins start accumulating in the gut region where the vagus nerve connects and spread into various brain regions gradually over time.
In addition, it has been found that surgical dissection of the vagus nerve causes inhibition of the translocation of misfolded proteins and reduction in nerve cell death.
Regarding behavioral changes related to Parkinson’s disease, the study has found that gut injection of misfolded alpha-synuclein in mice with intact vagus nerve causes a reduction in fine motor control and induction of anxiety-like behaviors.
Another study involving genetically modified, alpha-synuclein overexpressing rats have confirmed that misfolded proteins travel from the gut to the Parkinson’s disease-related brain regions via the vagus nerve, and the accumulation of pathological lesions in the brain increases with time.
Also, it has been found that apart from the brain, misfolded proteins can travel to the heart as well. This explains the presence of cardiac problems in patients with Parkinson’s disease.
Does Parkinson’s disease always originate in the gut?
A growing body of evidence suggests that patients with Parkinson’s disease may fall under two categories: the gut-first and the brain-first categories. In patients belonging to the gut-first subtype, the disease originates in the peripheral nervous system of the gut and eventually travels to the brain.
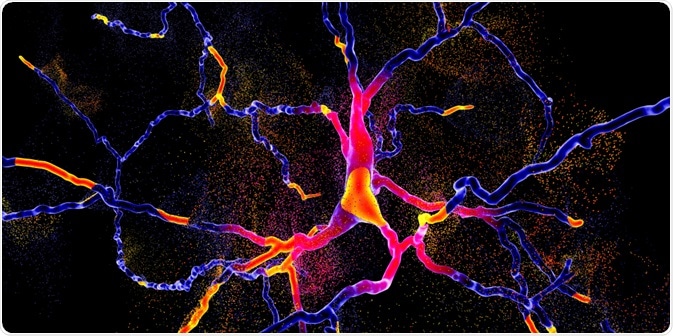
Image Credit: Kateryna Kon/Shutterstock.com
Whereas, in the brain-first subtype, the disease originates in the brain or enters the brain via the olfactory system and gradually spreads to the brainstem and peripheral nervous system.
As evidenced by the brain autopsy studies of Parkinson’s disease patients, some pathological lesions develop in the peripheral nervous system of the gut and nose and transmit to the brain.
However, in some cases, no lesions can be found in the brain’s entry point where the vagus nerve connects to the brainstem. This indicates that instead of coming from the peripheral nervous system, the disease is originated in the brain.
For the effective management of patients with Parkinson’s disease, it is important to evaluate the origin of the disease first. Treatments that are directed to the gut, such as probiotics, anti-inflammatory medicines, fecal transplants, etc., may not be effective in patients carrying the brain-first subtype of the disease.
Therefore, identification of the disease subtype and the development of personalized medicine are the two important steps to be considered for the effective management of Parkinson’s disease patients.
Last Updated: Apr 28, 2020