Skip to
Glioblastoma is the most common and aggressive type of adult brain tumor, and occurs in a variety of forms. At present, patients with a newly diagnosed tumor are advised to have surgery along with radiation and chemotherapy.
Despite the most energetic treatment using resection, where the diseased tissue is removed surgically, chemotherapy and radiation, patients typically do not live long. Less than two per cent of patients survive five years after diagnosis, the average length of survival is estimated to be only 12 to 15 months.
Patients under 45 years of age and those with a higher KPS (Karnofsky Performance Status) score before surgery, a method of scoring a patient’s functional impairment, have a slightly better prognosis. These patients are more likely to have a total resection (by postsurgical evaluation) and additional chemotherapy.
Glioblastomas result from abnormal growth of the glial cells which form a major part of the brain. In fact, they comprise 90% of brain cells. Glia are support cells of various types that provide mechanical strength and other vital elements to the neurons.
Most glioblastomas begin from a type of star-shaped glial cell called astrocytes, which help to make up the blood-brain barrier. Most glioblastomas begin in the frontal or temporal lobes of the brain, and spread in all directions. The ubiquity of glial cells in the brain make tumor spread easy and unpredictable.
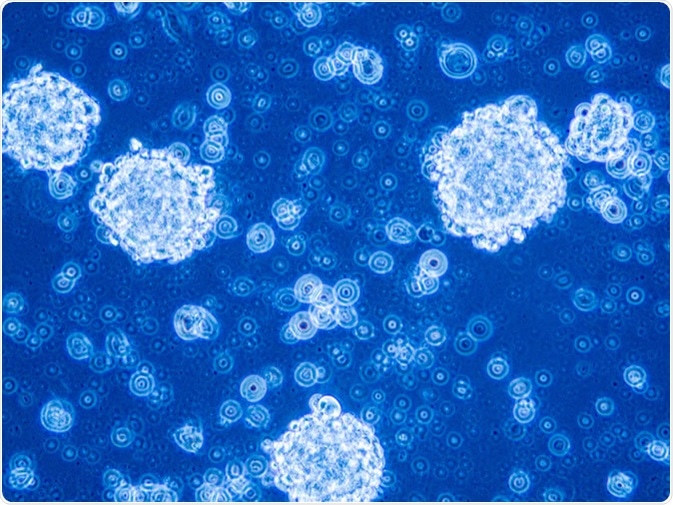
Glioblastoma stem cells organized in tumor niche formation. Image Credit: Anna Durinikova / Shutterstock
What happens when glioblastomas are resected?
Research has suggested that surgical resection of a glioblastoma causes the remaining part of the tumor to become more aggressive, resulting in a more rapid rate of growth of malignant cells into the space left by the resection. This is because of the normal events that occur during a wound healing response in any part of the body.
To investigate this process, the researchers allowed implanted glioblastoma cells to grow in mice to form symptomatic tumors. At this point they removed about 90% of the tumor, corresponding to the resection percentage typically achieved by neurosurgeons. On observation, they found that the tumor cells that were left behind grew around 75% faster than the average rate of growth before the surgery. The ratio of blood vessels to cells is also altered from that of the presurgical glioblastoma.
The researchers concluded that post-surgical tumor growth differed in some important ways from that of the primary tumor, and this was one of the reasons that recurrent glioblastomas were difficult to treat.
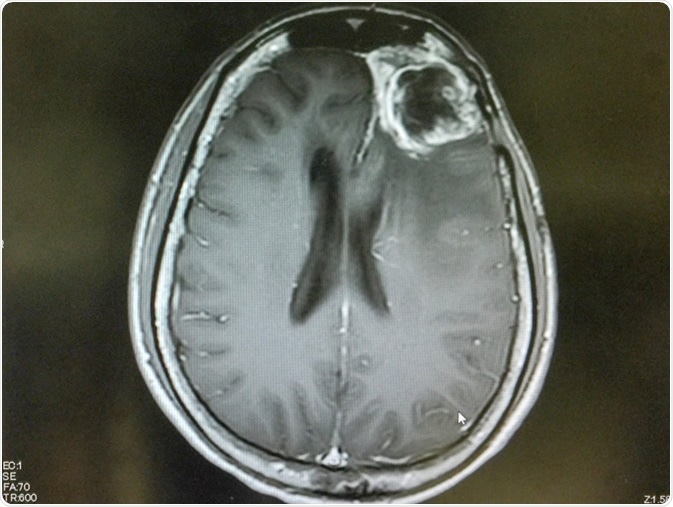
MRI brain show left frontal gliblastoma. Image Credit: O_Akira / Shutterstock
How does wound healing contribute to glioblastoma regrowth?
A simplified explanation for this phenomenon is that after removal of a large part of the tumor, normal astrocytes react to the removal of the healthy tissue which is inevitable with resection of cancers. The reactive astrocytes release multiple growth factors, which are chemicals produced by cells that encourage rapid multiplication and growth of tissue. These signals mediate compensatory cell growth, cell migration, and new vascular growth. As a result, the injured glial cells around the tumor cavity go into overdrive, proliferating to fill up the void as fast as possible.
In normal circumstances, these reactive astrocytes would form the glial scars that follow many types of brain injury. They produce high levels of proteins like glial fibrillary acidic protein (GFAP), which help to form the cytoskeleton. When these GFAP+ cells are in the vicinity of an invasive tumor, they pile up near the edges. These cells are affected by blunt force as a result of tumor resection. In response, they try to heal the perceived injury to normal tissue by expressing other proteins like nestin as well, which may cause them to behave more like stem cells, than mature glia.
The effect of these changes on tumor growth
Following surgery, the proportion of reactive astrocytes around the tumor, that is, the tumor microenvironment, is altered. The astrocytic growth signals are, unfortunately, also received and read by the cancerous glial cells, which also go into a frenzy of growth and migration. This leads to tumor progression as well as invasion of the surrounding area by malignant cells.
This research suggests that tumor resection is followed by reactive astrocyte response, which causes increased tumor proliferation and migration, increasing the grade of the malignant cells. The recurrent tumor is very invasive and grows faster than tumors that are not resected.
This research has proved vital in helping researchers understand how tumor biology alters after glioblastoma resection. More studies will be needed to identify the various factors involved in these changes. Ideally, this knowledge would assist the development of local treatments that can reduce the negative effects of surgery on tumor growth and invasion.
Further Reading
Last Updated: Aug 19, 2019