Introduction
Recent Developments
Why Experts Are Worried
How Prepared Are We?
Barriers to a Pandemic
What Needs to Happen Now
References
The rapid spread of H5N1 from wild birds to mammals, and even humans, is raising the stakes in the fight against avian influenza. As experts warn of the virus’s pandemic potential, global action on surveillance, vaccine development, and One Health strategies has never been more urgent.
 Image Credit: ShishkinStudio / Shutterstock.com
Image Credit: ShishkinStudio / Shutterstock.com
Introduction
H5N1, H5N6, and H7N9 are classified as highly pathogenic avian influenza viruses (HPAIVs) that belong to the influenza A genus. These viruses are characterized by surface proteins hemagglutinin (H) and neuraminidase (N), which determine their subtype and infectivity.2
H5N1 was first identified in 1959 in Scotland, with the first cases of human transmission reported almost 40 years later in Hong Kong. Between 2003 and 2023, the World Health Organization (WHO) documented 878 human cases of H5N1 infection with 458 deaths reported across 23 countries.
Viral transmission typically occurs through close contact with infected birds or contaminated environments. Although human-to-human transmission is rare, the ability of H5N1 to infect mammals, including cats, dogs, seals, and even sea lions, raises concerns about its evolutionary potential.2
The continued spread among wild and domestic bird populations globally, along with sporadic human infections, highlights bird flu as a persistent and evolving global health threat.
 Transmission of Highly Pathogenic Avian Influenza (HPAI) H5N1 to Humans, Birds, and Other Animals and The Action of Adaptive and Innate Immune Response against HPAI H5N1. Represent the activation of the innate immune response upon detection of HPAI H5N1 viral components. This response includes the release of pro-inflammatory cytokines, such as Interferons (IFNs), and the recruitment of innate immune cells. The adaptive immune response, including both the humoral and cellular immune responses, triggered by HPAI H5N1 infection. This response involves the activation and proliferation of antigen-specific B cells, resulting in the production of virus-neutralizing antibodies and the activation of T cells, including both cytotoxic T lymphocytes (CTLs) and helper T cells. The figure shows interactions between adaptive and innate immune cells, such as the presentation of viral antigens by antigen-presenting cells (APCs) to activate T cells and the cooperation between B cells and T cells for the production of specific antibodies.2
Transmission of Highly Pathogenic Avian Influenza (HPAI) H5N1 to Humans, Birds, and Other Animals and The Action of Adaptive and Innate Immune Response against HPAI H5N1. Represent the activation of the innate immune response upon detection of HPAI H5N1 viral components. This response includes the release of pro-inflammatory cytokines, such as Interferons (IFNs), and the recruitment of innate immune cells. The adaptive immune response, including both the humoral and cellular immune responses, triggered by HPAI H5N1 infection. This response involves the activation and proliferation of antigen-specific B cells, resulting in the production of virus-neutralizing antibodies and the activation of T cells, including both cytotoxic T lymphocytes (CTLs) and helper T cells. The figure shows interactions between adaptive and innate immune cells, such as the presentation of viral antigens by antigen-presenting cells (APCs) to activate T cells and the cooperation between B cells and T cells for the production of specific antibodies.2
Recent Developments
Between December 2024 and March 2025, HPAIVs spread across 31 countries, with 743 cases detected in birds, predominantly of the H5N1 subtype, including poultry, wild birds, and captive birds, with notable outbreaks in waterfowl like mute swans and geese.
The spread of H5N1 to mammals, including domestic cats and wild carnivores in Europe, as well as nearly 1,000 dairy cattle farms, has been reported in 17 U.S. states. A recent genetic analysis identified a different H5N1 genotype of D1.1 in U.S. cattle, which suggests potential viral evolution. Human infections remain rare but notable, with 22 new cases reported globally, including a U.S. dairy worker infected in 2024.3 Global health authorities, including the WHO and U.S. Centers for Disease Control and Prevention (CDC), are increasingly concerned about the potential for mutation and wider transmission of avian influenza. Although human-to-human transmission has not been observed, continued surveillance and precautionary measures remain critical due to the rapid geographic spread of this virus and its occasional ability to cross the species barrier.3
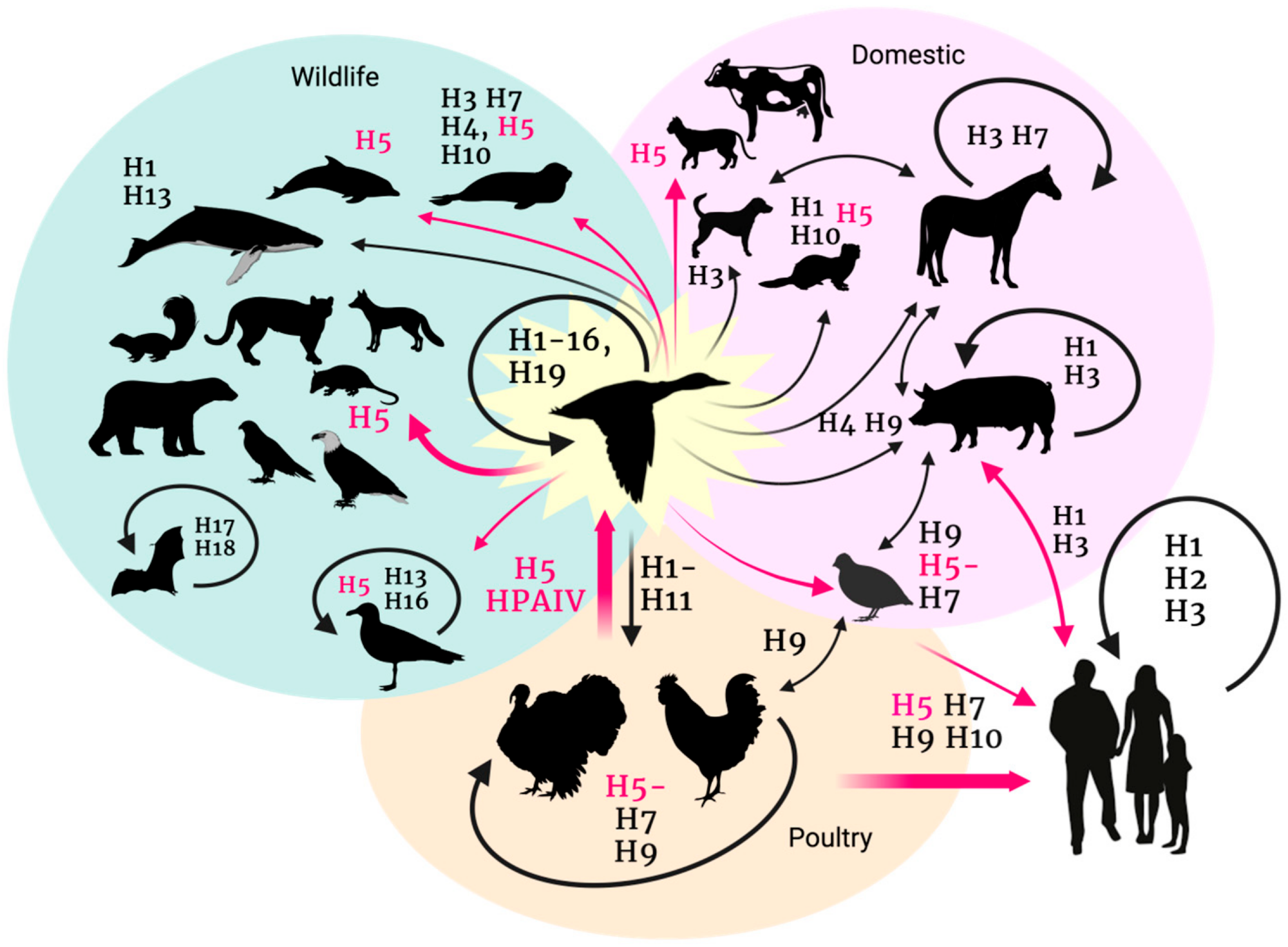 Avian influenza transmission flow from the natural reservoir (aquatic birds) to poultry, humans, and other animal species. Figure generated with BioRender.com8
Avian influenza transmission flow from the natural reservoir (aquatic birds) to poultry, humans, and other animal species. Figure generated with BioRender.com8
Why Experts Are Worried
Bird flu strains like H5N1 exhibit genetic flexibility that could eventually allow these viruses to infect mammals more efficiently. Recent cases of bird flu spreading among mammals such as minks, sea lions, and cows have raised fears that the virus could adapt to sustained mammal-to-mammal transmission, which increases the risk of a future pandemic.4
Unlike seasonal flu, which regularly circulates and allows populations to build partial immunity, avian strains remain largely unfamiliar to the human immune system. Furthermore, current human flu vaccines are not designed to protect against bird flu variants.4
Scientists warn what future bird flu mutations could mean for people | 60 Minutes
How Prepared Are We?
Surveillance systems for detecting avian influenza in birds, livestock, and humans exist in many countries. However, these strategies are often not equipped to identify outbreaks in unexpected species or under unusual circumstances. As a result, local reporting plays a crucial role in capturing early warning signs.
Although most strains of H5N1 are sensitive to antiviral drugs such as oseltamivir, clinical guidelines for treating avian influenza are limited and the available evidence remains weak. Stockpiling antivirals and personal protective equipment, as well as enhancing laboratory capacity, especially in lower-resource settings, is essential.5
Vaccine development infrastructure exists, with the WHO equipped with the capabilities needed to rapidly update candidate vaccine viruses in the event of an emergency situation. However, as evident during coronavirus disease 2019 (COVID-19) pandemic, equitable access and timely production of novel vaccines remain major challenges.
The early response to COVID-19 exemplifies the consequences of fragmented communication and uncoordinated actions. To avoid repeating these mistakes, global and national authorities must prioritize data sharing, rapid research, and clear communication between animal and public health sectors, ideally under a unified One Health framework.5
Stay current—read over 1,100 news stories on bird flu’s evolving global impact
Barriers to a Pandemic
Most human cases of bird flu arise from direct contact with infected birds, particularly during culling, handling, or live poultry markets. In these environments, especially in densely populated regions where humans and animals closely coexist, opportunities for interspecies transmission increase. Nevertheless, human-to-human transmission remains extremely rare and limited to isolated instances, which suggests that the virus is not well-adapted to human hosts.6
A single amino acid mutation in the H5 hemagglutinin protein can alter its receptor-binding properties, potentially allowing the virus to infect human cells more efficiently. This genetic shift could break existing species barriers.
Continuous monitoring of these mutations is crucial, as changes in the virus’s genome, particularly those affecting how it binds to human receptors, could eventually lead to sustained human transmission.6
What Needs to Happen Now
To reduce the risk of a bird flu pandemic, global disease monitoring systems must be strengthened to ensure early detection of outbreaks and viral mutations. This includes building and maintaining robust veterinary and public health surveillance infrastructures, especially in regions with close human-animal interaction.
Many developing countries lack the laboratory capacity and trained personnel needed for timely diagnosis and reporting of avian influenza in poultry and wild animals, which are primary reservoirs of the virus.
Existing human influenza vaccines offer limited protection against avian strains like H5N1 or H7N9; therefore, investing in bird flu-specific vaccine research and production is crucial.
Educating frontline workers, including farmers, animal health technicians, and veterinary professionals, is vital. Training programs can improve outbreak response, enhance biosecurity, and reduce the likelihood of animal-to-human transmission.7
References
-
Palù, G., Roggero, P. F., & Calistri, A. (2024). Could H5N1 bird flu virus be the cause of the next human pandemic? Frontiers in Microbiology, 15, 1477738. DOI: 10.3389/fmicb.2024.1477738, https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1477738/full
-
Charostad, J., Rezaei Zadeh Rukerd, M., Mahmoudvand, S., Bashash, D., Hashemi, S. M. A., Nakhaie, M., & Zandi, K. (2023). A comprehensive review of highly pathogenic avian influenza (HPAI) H5N1: An imminent threat at doorstep. Travel Medicine and Infectious Disease, 55, 102638. DOI: 10.1016/j.tmaid.2023.102638, https://www.sciencedirect.com/science/article/pii/S1477893923000984
-
Alexakis, L., Buczkowski, H., Ducatez, M., Fusaro, A., Gonzales, J. L., Kuiken, T., Ståhl, K., Staubach, C., Svartström, O., Terregino, C., Willgert, K., Melo, M., & Kohnle, L. (2025). Avian influenza overview December 2024–March 2025. EFSA Journal, 23(4), e9352. DOI: 10.2903/j.efsa.2025.9352, https://efsa.onlinelibrary.wiley.com/doi/abs/10.2903/j.efsa.2025.9352
-
Dey, P., Ahuja, A., Panwar, J., Choudhary, P., Rani, S., Kaur, M., Sharma, A., Kaur, J., Yadav, A. K., Sood, V., Suresh Babu, A. R., Bhadada, S. K., Singh, G., & Barnwal, R. P. (2023). Immune Control of Avian Influenza Virus Infection and Its Vaccine Development. Vaccines, 11(3), 593. DOI: 10.3390/vaccines11030593, https://www.mdpi.com/2076-393X/11/3/593
-
Kojima N, Adlhoch C, Mitja O, Dat VQ, Lescano AG, Klausner JD. Building global preparedness for avian influenza. Lancet. 2024 Jun 8;403(10443):2461-2465. DOI: 10.1016/S0140-6736(24)00934-6. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)00934-6/fulltext
-
Mittal N, Medhi B. The bird flu: a new emerging pandemic threat and its pharmacological intervention. Int J Health Sci (Qassim). 2007 Jul;1(2):277-83. PMID: 21475439; PMCID: PMC3068632, https://pmc.ncbi.nlm.nih.gov/articles/PMC3068632/
-
Jonas, O., & Warford, L. (2014). Global program for Avian Influenza control and human pandemic preparedness and response: project accomplishments. Health, Nutrition and Population (HNP) Discussion Paper Series, (94043) https://documents1.worldbank.org/curated/en/527421468329073537/pdf/940430WP0Box385430B0GPAI0Final00PUBLIC0.pdf
-
Graziosi, G., Lupini, C., Catelli, E., & Carnaccini, S. (2023). Highly Pathogenic Avian Influenza (HPAI) H5 Clade 2.3.4.4b Virus Infection in Birds and Mammals. Animals, 14(9), 1372. DOI: 10.3390/ani14091372, https://www.mdpi.com/2076-2615/14/9/1372
Last Updated: May 27, 2025