Antibody-drug conjugates allow the targeted delivery of a specific drug dose to the site of interest. They are most commonly employed in oncology, where a high drug dose is required at the tumor site, but not the surrounding tissue.
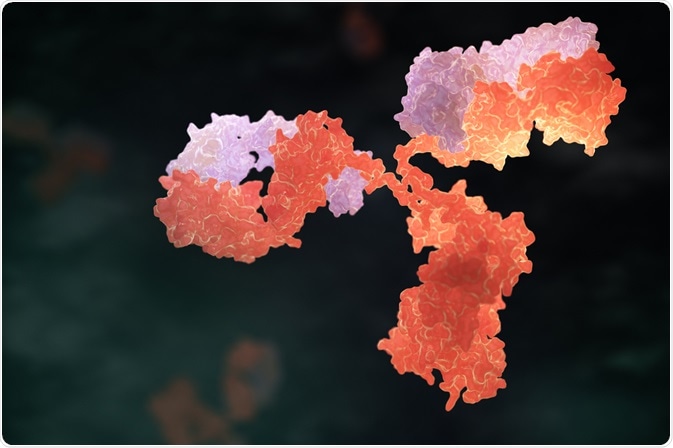 Image Credit: Tatiana Shepeleva / Shutterstock
Image Credit: Tatiana Shepeleva / Shutterstock
Biopharmaceutics is a rapidly growing research field that aims at producing viable therapeutic and prophylactic treatments for many diseases.
The use of biological therapies has increased exponentially, especially in the treatment of cancer. However, the use of biological agents alone showed limited clinical efficacy.
For instance, prolonged administration of chemotherapy with cytotoxic agents may cause severe cytotoxicity and drug resistance.
As a result, researchers started focusing on the use of targeted therapy in conjugation with small drug molecules to enhance the efficiency of potent drugs. This is where antibody-drug conjugates (ADCs) come into play.
Structure and pharmacological action of ADCs
ADCs have three parts namely the antibody, linker, and the drug. The pharmacological action of ADCs is divided into four steps; action on the systemic circulation, enhanced permeability and retention (EPR) effect, tumor tissue penetration, and active targeting of cells with sustained release of drug. The linker part of the ADC is responsible for sustained drug release.
This targeted approach of ADCs encourages selective attack of malignant cells only. It also improves patient outcomes with fewer episodes of adverse events than what is observed with conventional chemotherapeutic methods.
History and development of ADCs
In 1913, Paul Ehrlich, a German physicist and scientist, was the first to propose the concept of targeted delivery of toxic agents against microbes or tumor cells.
It took almost four decades of research to bring about a promising outcome of ADCs in clinical trials. The first successful ADC clinical trial was in 1983 that used an anti-carcinoembryonic antigen antibody-vindesine conjugate.
In the 1990s, the first-generation ADCs were derived from the backbones of murines. However, the linkers were not stable in the human blood stream because of which the ADCs had a short half-life.
In addition, the concentration of the cytotoxic agent (also referred to as cytotoxic payload) was minimal.
Only 1-2% of the dose reached the tumor site and this did not offer the required therapeutic efficacy in humans. Subsequently, clinical trials were stopped due to non-efficacy of these first-generation ADCs.
Around the same time, an FDA-approved ADC used to treat acute myeloid leukemia was discontinued owing to fatal adverse events because of an unstable linker that led to premature release of the cytotoxic payload.
ADCs pose challenges due to their complex structure and have some limitations such as low chemotherapeutic potency and antigen selectivity.
Despite numerous setbacks encountered while developing ADCs, rapid progress is being made due to technological advancements such as antibody engineering to introduce novel linkers or site-specific conjugation chemistry to improve the outcome of ADCs.
For instance, strategic linker designs with enhanced hydrophilicity can be used in multi-drug resistant tumors to reduce binding of the payload in ADCs.
What are Antibody-drug Conjugates (ADCs)?
FDA-approved antibody-drug conjugates
Several ADCs are FDA-approved for the treatment of refractory Hodgkin’s lymphoma and HER2-positive breast cancer.
Currently, ADC research is making use of fluorescent imaging, positron emission tomography (PET), and magnetic spectrometry imaging (MSI) to evaluate antibody delivery and sustained drug release.
There are 60 ADCs undergoing clinical trials of which some trials are even using combination strategies such as ADCs with conventional chemotherapy.
Addressing molecular designs and strategies to produce effective and safe ADCs can pave the way for novel biological therapeutics.
Further Reading
Last Updated: Aug 30, 2018