Antibody engineering describes the production of human antibodies using in vitro or in vivo techniques for research or clinical use. Since its inception, antibody engineering has grown to encompass a range of production technologies and techniques.
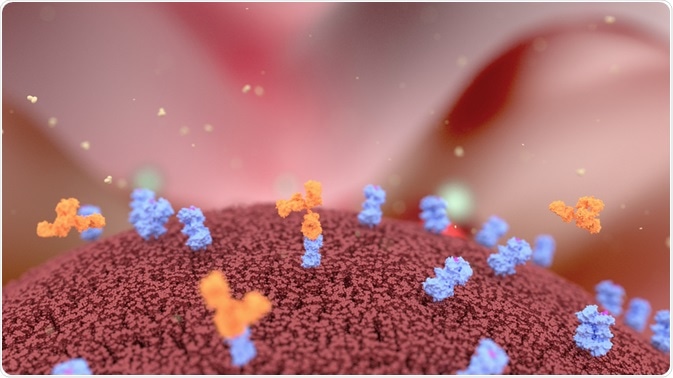
Alpha Tauri 3D Graphics | Shutterstock
What are antibodies?
Antibodies are naturally occurring proteins associated with the immune system with a primary task to identify and neutralize threats, such as bacteria and viruses. They are capable of recognizing specific protein patterns, which makes them useful in clinical diagnostic and therapeutic domains.
The first engineered antibodies were approved for marketing by the US Food and Drug Administration (FDA) in 1997. These were monoclonal antibodies from mice that bound to tumor-specific antigens and could, therefore, differentiate cancer cells from healthy cells.
Since then, around 300 programs for the development of therapeutic antibodies have been described in industrial and academic laboratories.
The development of antibodies is now a central approach to combating several notable pathogenic diseases. They can defend against transmissible diseases or completely eliminate an infection.
Polyclonal antibodies contain varying concentrations of different antibodies, and as such are not commonly used clinically. Conversely, monoclonal antibodies are highly specific, permitting more enhanced clinical diagnostics.
How to approach antibody engineering
Active production of human antibodies started after the realization that transgenic mice could be developed and used, which are experimental animals that contain some human genes in their genome. More specifically, in the case of antibody engineering, they contain human antibody gene sequences.
In vitro generation followed this, using antibody engineering techniques such as phage display, construction of antibody fragments, immunomodulatory antibodies, and cell-free systems. This allowed true engineering endeavors to carefully select genetically engineered recombinant libraries using phage display technology.
The first human monoclonal antibody was engineered using phage display and choosing antigen-specific binders from blood lymphocyte libraries. The transgenic animals used, mice and rabbits, were integrated with human immunoglobulin loci.
Other therapeutic solutions utilizing small molecules have sometimes failed where engineered antibodies have succeeded. Engineered monoclonal antibodies are capable of binding with high affinity and high specificity to molecular targets that are classically seen in diseased conditions, but absent in normal cells.
Where the specific action is known, engineered antibodies work using several known activities.
- First, they can work by antagonistic action by hindering an interaction between a cell receptor and its ligand.
- Secondly, antibodies can recruit immune cells to the target tissue by their Fc domain, to initiate antibody-dependent cellular cytotoxicity (ADCC) or complement-dependent cytotoxicity (CDC).
- Thirdly, they can induce apoptosis via receptors, and modulate the expression of cell-surface receptors.
- Lastly, conjugated antibodies (antibodies bound to a therapeutic drug) can aid the delivery of radioisotopes or chemotherapeutic drugs to the site of interest, minimizing side effects and maximizing efficacy.
Pertinent challenges
Engineered antibodies rely on knowledge about molecular targets, and therefore their progress is limited to known receptors.
Recent technological innovations, such as genome sequence compilations and new advances in understanding cell signaling, have provided a high number of novel potential targets for antibody development. These are especially prevalent in oncology, such as agonistic antibodies targeting the human tumor necrosis factor related apoptosis-inducing ligand receptor (TRAIL).
At present, engineered antibodies are limited by their ability to bind only extracellular receptors, ligands, and other blood proteins. Thankfully, many signaling proteins act at the cell surface or extracellular environment.
While antibody engineering has grown, it has also had serious shortcomings. In one case, a phase I clinical trial in the UK resulted in six healthy participants being admitted to intensive care. The antibody in question targeted CD28 to activate T cells, with the hope of targeting autoimmune diseases. This has pushed the industry to be more careful and vigilant in selecting and engineering antibodies for human use.
What does the future hold for antibody engineering?
The majority of engineered monoclonal antibodies currently at some stage of clinical trials are owned by small biotechnological companies. This may be expected to change, given the large revenues and approval ratings that by far exceed those of other small molecule drugs.
As of 2005, 18 therapeutic monoclonal antibodies were approved by the FDA. Of those, 89% are related to oncological or immunological treatment. Following this trend, the majority of therapeutic monoclonal antibodies being considered for clinical use belong to three main areas of potential targeted treatment: oncological, immunological and anti-infective.
Further Reading
Last Updated: Apr 6, 2023