A B cell is a type of white blood cell or lymphocyte that is part of the vertebrate adaptive immune system. B cells secrete antibodies in response to invasion by foreign pathogens.
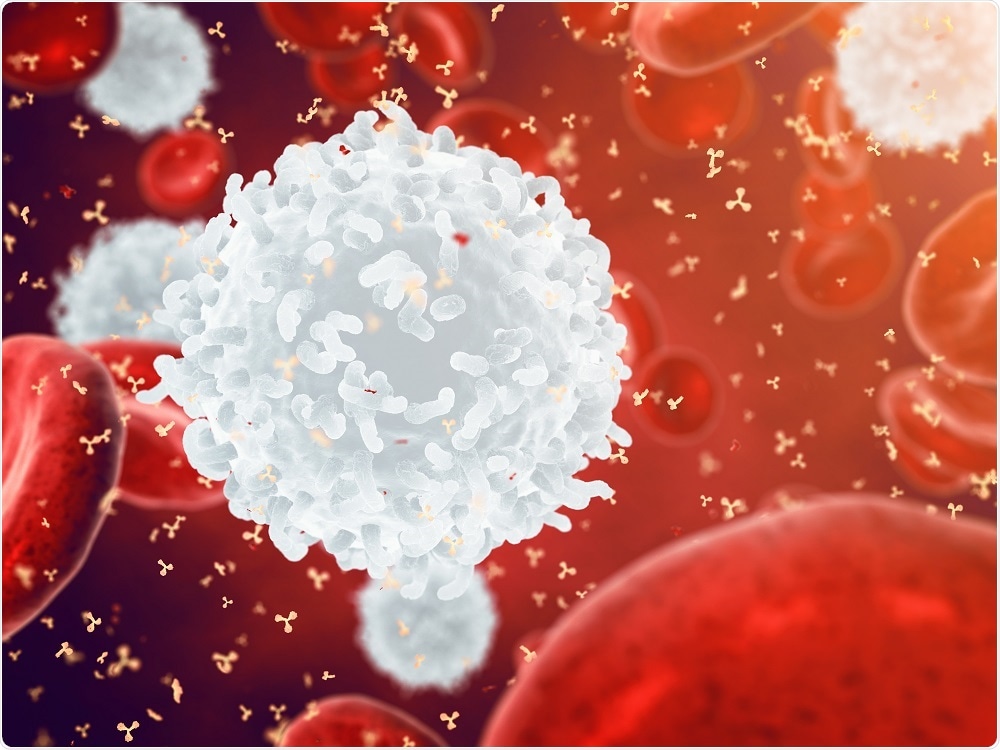 Credit: nobeastsofierce/Shutterstock.com
Credit: nobeastsofierce/Shutterstock.com
B cells originate in fetal liver and bone marrow in mammals, developing from hematopoietic stem cells (HSCs). HSCs become multipotent progenitor (MPP) cells, then common lymphoid progenitor (CLP) cells, and then go through several more stages of development to become a mature B cell.
Multipotent hematopoietic progenitors of B cells migrate into the fetal liver and bone marrow, and take up residence in new environments to commence development along the B lineage pathway. Initially, rearrangements of genes generate precursors that express IgH antibodies. When IgH is able to pair with an IgL light chain, a pre-B cell receptor is formed.
In the next stage, autoreactivity of the IgH chain is interrogated. Then IgM is displayed as a B cell receptor on the immature B cells, and these cells are presented with autoantigens.
Those with high-affinity autoreactive B cell receptors are deleted, and those with low-affinity autoreactive B cell receptors leave the bone marrow and enter peripheral blood pools, particularly in the lung and gut lymphoid tissues.
More than 85% of new, immature B cells die in the bone marrow due to autoantigen recognition. This process generates central tolerance to autoantigens. More detailed characterization of autoantigen presentation occurs at later stages of development.
In the spleen, B cells are monitored in transition from immature to mature cells. Mature B cells in the peripheral blood are tested for their ability to recognize foreign antigens.
B cells that respond are propagated and undergo a process called hypermutation, where their genes are rearranged to create a B cell receptor that better fits the foreign antigen. B cells that become autoreactive through the hypermutation process and are not destroyed can lead to autoimmune disease.
Microenvironment of the bone marrow
The bone marrow microenvironment crucially shapes the development of B cells. Bone marrow stromal cells create distinct niches that support B cell development.Factors required for B cell development are thought to be produced by cells of the bone marrow, and are delivered to the precursor B cells at an appropriate stage of development.
Reticular cells, surrounding bone marrow sinuses, have been shown to be associated with B cells, and may play a role in forming niche environments for B cell development. Other cells that may provide cellular niches include osteoblasts and IL-7 expressing cells.
B cell activation
B cells are activated in the secondary lymphoid organs (SLOs), which are the lymph nodes, tonsils, spleen, Peyer's patches and mucosa associated lymphoid tissue (MALT). Upon maturation, B cells migrate to the SLO.
The SLO receives a steady supply of antigens through circulating lymph. B cells are activated when they bind to an antigen through a B cell receptor. The surface receptor CD21 can enhance B cell activation in complex with CD19 and CD81.
In that process, the B cell receptor binds an antigen tagged with a fragment of C3 complement protein, and CD21 binds the fragment. It then co-ligates with the bound B cell receptor and a signal transduction cascade is initiated that lowers the activation threshold of the cell.
B cells can also undergo T cell dependent activation, which occurs when a B cell receptor binds a T cell-dependent antigen. The antigen is then taken up into the B cell and presented to T cells on the cell membrane.
A T helper cell activated with the same antigen recognizes and binds the antigen complex, triggering a cascade of signals. Once the B cells receive the signals, they are activated, and undergo a two-step differentiation resulting in short-lived plasmablasts for immediate response and long-lived plasma cells and memory B cells for long term response.
Further Reading
Last Updated: Feb 26, 2019