Gram staining is a type of differential staining used to distinguish between Gram positive and Gram negative bacterial groups, based on inherent differences in their cell wall constituents.
 Credit: fusebulb/Shutterstock.com
Credit: fusebulb/Shutterstock.com
Stains increase contrast allowing bacteria to be observed with greater ease.Gram staining is dependent on the interaction between the negatively charged surface of bacteria and the positive ions within common stains.
Gram negative bacteria are often pathogenic and contain endotoxins within their outer membranes. The cell wall structure of Gram negative bacteria also confers an increased ability to resist antibiotics. Escherichia coli is an example of a common Gram negative bacterium.
Gram stain procedure
The Gram stain procedure was developed by Hans Christian Gram in the 1800s and was one of the first techniques taught to students in microbiology laboratories. A dried bacterial smear is flooded with a crystal violet stain before iodine is added to fix the stain into an insoluble complex.
The smear is de-stained using an alcohol or acetone solution to remove any weakly bound stain, before being counterstained with the red dye, safranin. The slide is rinsed between each procedural step with the final wash acting as preparation for observation under a microscope.
Gram positive bacteria are observed as blue or violet colored cells (having retained the stain) whilst Gram negative bacteria appear pink because of the counterstain.
Gram negative bacteria cell wall structure
Gram negative bacteria are characterized by the presence of the periplasmic space, which is a single layer of peptidoglycan sandwiched between the cytoplasmic membrane and the outer membrane. Peptidoglycan, also known as murein, is a polymer that consists of a carbohydrate backbone and amino acids.
Peptide chains within the peptidoglycan structure are partially cross-linked in Gram negative bacteria, contrasting with the highly cross-linked peptide chains of Gram positive bacteria.
The outer membrane contains lipopolysaccharide, a large molecule that is toxic to animals. During Gram staining, the outer membrane of Gram negative bacteria deteriorates from the alcohol added to the sample and the thin layer of peptidoglycan is not able to retain the crystal violet stain.
The counterstain is added to provide contrast by staining the decolorized Gram negative bacteria through the thin peptidoglycan layer whilst being light enough to not disturb the crystal violet staining on the Gram positive bacteria.
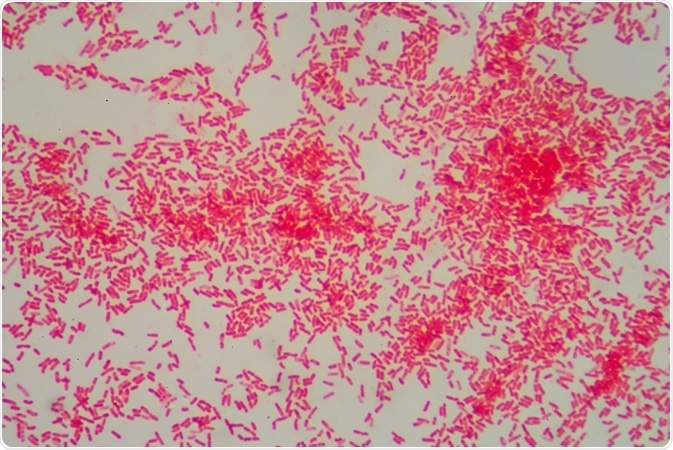 Credit: toeytoey/Shutterstock.com
Credit: toeytoey/Shutterstock.com
Gram negative bacteria as pathogens
Gram negative bacteria are often pathogenic and include Escherichia coli, a common cause of food poisoning and Vibrio cholerae, the waterborne pathogen responsible for cholera outbreaks. The pathogenic capability of Gram negative bacteria is caused by their constituent membrane components.
The lipopolysaccharide endotoxin that resides in the outer membrane can cause a toxic reaction or strong immune response in the host animal. Gram-negative bacteria that enter the circulatory system may release lipopolysaccharides in large enough amounts to trigger an immune response that is injurious to the host’s organs and tissues.
The circulating lipopolysaccarides found within the blood stream of patients suffering from sepsis indicates that endotoxins are an important drug target for the prevention and treatment of septic shock.
Gram negative bacteria and resistance to antibiotics
Gram- negative bacteria are less susceptible to antibiotics because of their outer membrane. This is because the outer membrane provides protection from treatments that would ordinarily damage the inner membrane. Antibiotic resistant strains of bacteria have been noted to display modifications in the lipid or protein composition of the outer membrane.
Small hydrophilic antibiotics target porins, protein channels that provide a pathway through the outer membrane. Antibiotic resistance has been linked to a reduction in the rate of entry for antibiotics through porins via modifications to the outer membrane profile or reduced permeability caused by specific mutations.
Reviewed by Gillian D’Souza, MSc
Sources:
- Beveridge, T.J. 2001. Use of the gram stain in microbiology, Biotechnic and Histochemistry, 76, pp. 111-118.
- National Institute of Allergy and Infectious Disease: Gram-negative bacteria.
- Opal, S.M. & Glück, T. 2003. Endotoxin as a drug target, Critical Care Medicine, 31, pp. 57-64.
- Delcour, A.H. 2009. Outer membrane permeability and antibiotic resistance, Biochimica et Biophysica Acta, 1794, pp. 808-816.
Further Reading
Last Updated: Aug 23, 2018