Introduction
What types of nanoparticles can be administered by the pulmonary route?
How are nanomedicines designed to purpose?
References
Inhalation-based administration of drugs and therapeutics is commonly encountered in treating pulmonary diseases, being relatively non-invasive and allowing direct delivery to the site of action, possibly also avoiding systemic side effects that would result from greater circulation in the blood if delivered intravenously. The high surface area and dense vasculature of the lungs allow rapid perfusion of the therapeutic into local tissue and the general bloodstream if desired, where penetration can be controlled by careful nanomedicine design, also allowing the medicine to avoid the detrimental environment of the gastrointestinal tract as encountered during oral delivery.
Inhaled therapeutics are typically in a water droplet aerosol form or might be delivered as a fine dry powder, though the delivery of raw free drugs in powder form is frequently limited by local toxicity and poor retention around the site of disease. Additionally, many drugs are poorly water-soluble and cannot be aerosolized, and thus nanoparticle delivery systems have been investigated to aid the passage of inhaled therapeutics and mitigate off-target effects.
Image Credit: Volodymyr Horbovyy/Shutterstock.com
What types of nanoparticles can be administered by the pulmonary route?
Nanoparticle delivery systems are being increasingly adopted for many specific applications in medicine, those constructed from liposomes recently seeing widespread use in the delivery of sensitive mRNA coding for the SARS-CoV-2 spike protein in COVID-19 vaccines. As one of the most extensively investigated and utilized nanocarrier systems, liposomes have been explored in delivering various drugs intended to treat pulmonary issues, and several reach the clinic.
Alveofact is a liposomal formulation consisting of natural bovine lung surfactant delivered in aerosol form and administered to treat acute respiratory distress syndrome. As the liposomes themselves can be constructed from lung surfactant molecules, issues surrounding biocompatibility are avoided, and the liposomes can further still be loaded with drugs and other therapeutic or diagnostic agents.
Nanoparticles constructed from polymers and solid lipids can also be highly biocompatible and are suitable for nebulization or preparation as a dry powder. In particular, polymers exhibit better stability than lipid-based systems during storage and nebulization. Inorganic nanoparticles constructed from iron oxide, gold, or silver have more frequently demonstrated toxicity towards lung tissues when delivered by inhalation, largely by the generation of reactive oxygen species, though adverse effects may be controlled with low doses and controlled exposure. Such nanoparticles serve a different purpose as diagnostic agents, acting as contrast enhancers for X-ray imaging or magnetic resonance imaging in the case of iron oxide nanoparticles.
Nanoparticles, in general, can be loaded with active targeting molecules on their expansive surface area that heavily favors uptake into the desired cell type, for example where a tumor is significantly over-expressing a particular surface receptor, a nanoparticle may be decorated with the complimentary protein, allowing the precise dimensions of the tumor to be determined when acting as a diagnostic agent.
Several types of nanoparticles are suitable for delivery into the lungs by nebulization or as a dry powder, though extremely small and light nanoparticles with a maximum dimension in the sub-100 nm range take a very long time to settle in air and, as a result, a large portion of the dose may be exhaled when delivered as a dry powder. Therefore, where nebulization is not an option, dry powder agglomerations of nanoparticles on the micron scale are utilized for deep lung delivery.
How are nanomedicines designed to purpose?
The construction material of nanoparticles, along with other physicochemical properties, determine the distribution of an inhaled carrier within the lungs as well as systemically if absorbed into the bloodstream. For example, larger particles tend to deposit in the respiratory tract due to quicker sedimentation by gravity, while smaller particles remain suspended for longer and better reach the deeper regions of the lungs.
Once inhaled, nanoparticles settle onto the adhesive mucus lining the lungs, continuously moving up the mucociliary escalator to be swallowed or coughed up. Mucus and the mucociliary escalator represent a possible impediment to nanoparticles, which must penetrate the mucus to make contact with the epithelial cells and ultimately reach their target site.
Interestingly, the albumin and lecithin in the alveolar epithelial lining are essential to facilitate epithelial nanoparticle uptake, and particles coated with these proteins are better taken up. Nanoparticles that remain in the mucus and escape the mucociliary escalator are primarily cleared from the lungs by alveolar macrophages, though some studies show that retention periods can be very long, in the order of years, and macrophages fail to phagocytose smaller particles that comparatively stimulate fewer surface receptors.
In some disease states, the macrophages are the therapeutic target, and thus utilizing larger nanoparticles that they better take up constitutes a valid targeting strategy, though toxicity issues associated with long-term accumulation of nanoparticles in the lungs limit the applicability of particles that evade excretion too completely.
Besides traditional small molecule drugs, protein and gene therapeutics that would otherwise quickly degrade can be bound with nanocarriers and enter cells locally. Nanocarriers carrying all forms of therapeutics have been most widely explored by intravenous delivery, allowing the particles direct access to the systemic circulation and imposing fewer barriers towards circulation, though pulmonary delivery presents several advantages for certain applications.
Where the ultimate delivery target is the lungs, the advantages of direct inhalation are obvious, though some drugs intended for systemic biodistribution also benefit from pulmonary delivery. For example, insulin demonstrates a faster mechanism of action when delivered via the lungs than by injection, and penetration through the physical and chemical barriers discussed is aided by conjugation with polymer nanoparticles.
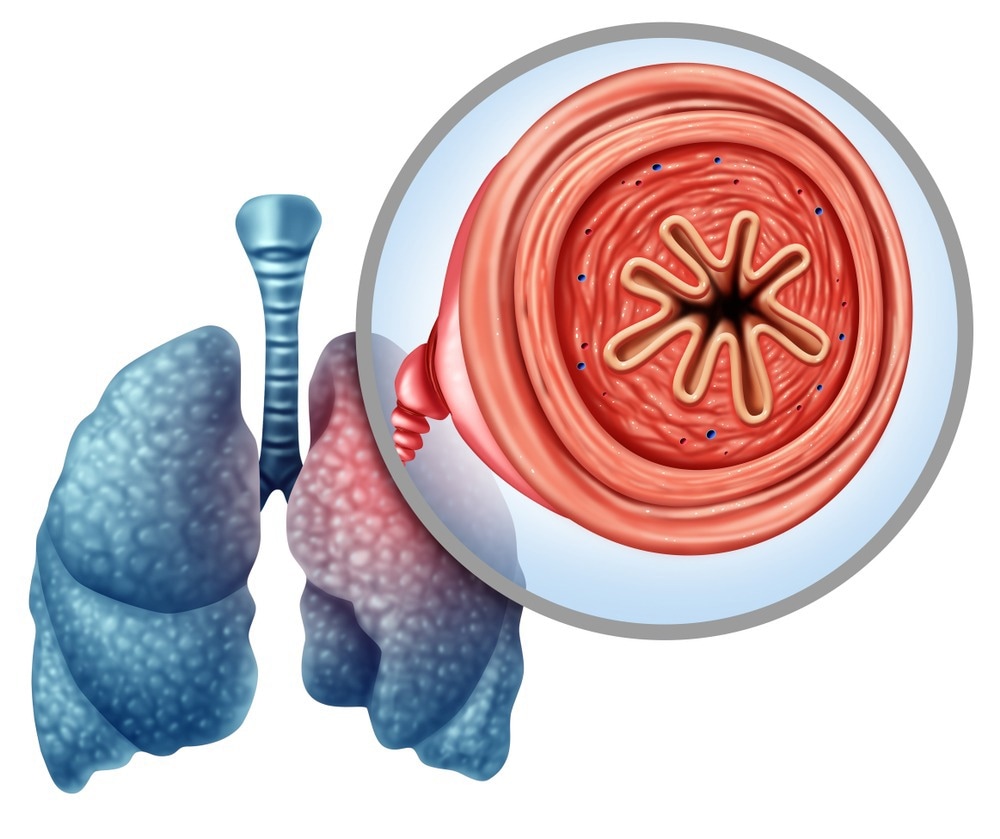
Image Credit: Lightspring/Shutterstock.com
References:
- Anderson, C. F., Grimmett, M. E., Domalewski, C. J., & Cui, H.. (2020). Inhalable nanotherapeutics to improve treatment efficacy for common lung diseases. Wires Nanomedicine and Nanobiotechnology, 12(1). https://doi.org/10.1002/wnan.1586
- Mansour, H., Haemosu, & Wu, X.. (2009). Nanomedicine in pulmonary delivery. International Journal of Nanomedicine, 299. https://doi.org/10.2147/ijn.s4937
- Mansoor, S., Kondiah, P. P. D., Choonara, Y. E., & Pillay, V.. (2019). Polymer-Based Nanoparticle Strategies for Insulin Delivery. Polymers, 11(9), 1380. https://doi.org/10.3390/polym11091380
- Van Rijt, S. H., Bein, T., & Meiners, S.. (2014). Medical nanoparticles for next generation drug delivery to the lungs. European Respiratory Journal, 44(3), 765–774. https://doi.org/10.1183/09031936.00212813
Further Reading
Last Updated: Feb 7, 2023