Recent studies have uncovered that specific genes are crucial at various stages of spermatogenesis, which may serve as biomarkers of male infertility.
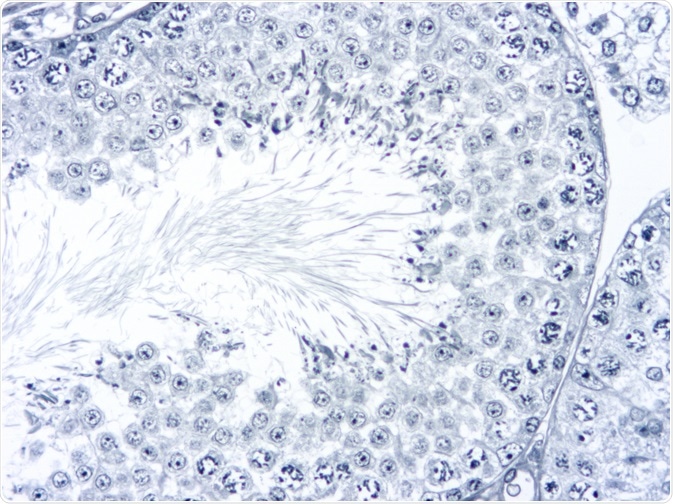
Image Credit: Tinydevil/Shutterstock.com
Genes related to spermatogenesis linked with infertility
Evidence has led experts to believe that genetics may be accountable for the difficulties that a significant portion of couples face when trying to conceive a child. Because men are just as likely to be the cause of fertility problems as women are, it is essential to uncover the genetic biomarkers that are associated with infertility to help improve the outcome of fertility treatments.
Studies have elucidated that there are differences in the gene expression profiles of fertile and infertile men. Many of these genes are related to the process of spermatogenesis, meaning that these associated genes may serve as male fertility biomarkers.
Further to this, studies in the past decade have also supported the use of microarrays as a potential diagnostic platform for male infertility and may be used as part of a treatment process.
What is spermatogenesis?
The process of spermatogenesis is the formation of sperm cells within the testes. The sperm is produced in the seminiferous tubules of the testis, and develop from germ cells. Mitotic division of spermatogonial stem cells is the first stage of the process, which results in the creation of type A cells, and type B cells.
Type B are those that differentiate into spermatocytes. These then divide meiotically, forming secondary spermatocytes that divide again into two haploid spermatids. This is where the cells are then converted into sperm cells through the process of spermiogenesis, the final phase. Genes related to different phases of this process are related to male infertility.
Microarrays discover critical genes for spermatogenesis
Back in 2002, a study was published that was one of the first to use microarray analysis on the genes expressed in the human testes. The investigations showed that the microarray technique could be appropriately applied to generating gene expression profiles of the testes.
Furthermore, they helped to identify the crucial genes playing a role in the testes and spermatogenesis, also, they were able to uncover the transcriptomes that are fundamental to the various stages of spermatogenesis. This opened up the possibility of using those genes as potential biomarkers.
Essential genes involved in spermatogenesis
As outlined above, there are several distinct phases of spermatogenesis, mitotic, meiotic, and post-meiotic. Profiles of gene expression are distinct to each of these phases.
Studies have shown that genes from DAZ family and TSPY1 are essential during the premeiotic and meiotic stages, whereas PRM2, TNP1, SYNJ2, and ZPBP were key to the postmeiotic stage. Further studies have been able to identify that genes involved in mitosis, the cell cycle, and specific genes such as IDE and RAN are also highly expressed, and essential to spermatogenesis. Also, it has been found that genes involved in the activation of kinases, signal transduction, and the organization of the cytoskeleton were also highly expressed during the post-meiotic stage.
These studies have been key in determining which genes are essential at the different stages of spermatogenesis, opening up the possibility of using them as biomarkers of not just infertility, but infertility type.
Potential biomarkers identified for male infertility
Various studies using microarray analysis have confirmed a link between several different genes, whose involvement in spermatogenesis is key, to the causes of infertility. These genes have been categorized in relation to their function, such as cell cycle regulation, cell metabolism, germ cell development, and chromatin remodeling, as well as a group of genes that have been left uncategorized due to their expression in all stages of spermatogenesis.
The identification of these genes has helped scientists to understand the genetic involvement throughout different stages of spermatogenesis, demonstrating how genes can be responsible for maladaptive processes at key moments, leading to fertility problems.
Sertoli cell-only syndrome is a condition where the seminiferous tubules in the testes only hold Sertoli cells, “nurse” cells that assist in the production of sperm, causing infertility. Studies have shown that patients with this condition do not express the PKH-T gene, also, the DAZ, SYNJ2, TSPY1, CDC25c, CLGN, BRDT, and PRM2 genes have been implicated in Sertoli cell-only syndrome. These genes have become potential biomarkers for male infertility.
Implications of spermatogenesis biomarkers
Given that around 15% of couples trying to conceive struggle with infertility, and the ‘male factor’ and ‘female factor’ account for this equally, half and half, research that elucidates the causes of male infertility are fundamental to assisting a significant portion of the population.
Spermatogenesis, the creation of sperm, is crucial to being able to conceive. The above-discussed research that has uncovered the specific genes involved in this process, and which genes are responsible for the distinct stages of this process, has helped scientists to understand the root problems causing male infertility.
These identified genes can potentially be used as biomarkers for male infertility, which could help to increase the diagnostic accuracy of male infertility, as well as inform new therapeutic techniques.
Sources:
Ibtisham, F., Wu, J., Xiao, M., An, L., Banker, Z., Nawab, A., Zhao, Y. and Li, G. (2017). Progress and future prospect of <i>in vitro</i> spermatogenesis. Oncotarget, 8(39). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5630449/
Kurpisz, M., Waclawska, A., Rozwadowska, N., Stokowy, T., Kolanowski, T., Jedrzejczak, P. and Zietkowiak, W. (2014). Novel gene biomarkers of spermatogenesis - the potential for spermatogenesis assessment and treatment monitoring. Fertility and Sterility, 102(3), p.e349. https://www.fertstert.org/article/S0015-0282(14)01806-8/abstract
Waclawska, A. and Kurpisz, M. (2012). Key functional genes of spermatogenesis identified by microarray analysis. Systems Biology in Reproductive Medicine, 58(5), pp.229-235. www.tandfonline.com/doi/full/10.3109/19396368.2012.693148?src=recsys
Further Reading
Last Updated: Feb 3, 2020