The American Cancer Society (ACS) reported that 1 in 8 women will be diagnosed with breast cancer in her lifetime. There are almost 14 million new cases diagnosed and approximately 4.5 million deaths related to a breast cancer diagnosis each year. As the most common cancer diagnosed in women, efficient detection is highly important.

Breast cancer screening. Image Credit: Gorodenkoff/Shutterstock.com
Breast Cancer
Breast cancer is extremely varied in its presentation, with some tumors having a slow growth rate and a good prognosis and others being highly aggressive. An early diagnosis is very important and recent advances in screening and detection have made it possible to start treatment earlier and give the patient the best possible chance of survival.
The wide variety in the presentation of breast cancer tumors is due in part to variation in the tumor structure and cellular components. It is also thought to be due to differences in specific biomarkers and variations in patient age, race, and lymph node function. The menopause is also thought to influence the presentation of the tumor.
Although there have been major breakthroughs in both technical and medical advances in recent years, there has been an 18% increase in cases diagnosed and related deaths between 2008 and 2012. This could be due to a poor understanding of some of the underlying mechanisms present in particularly aggressive forms of cancer.
Classification
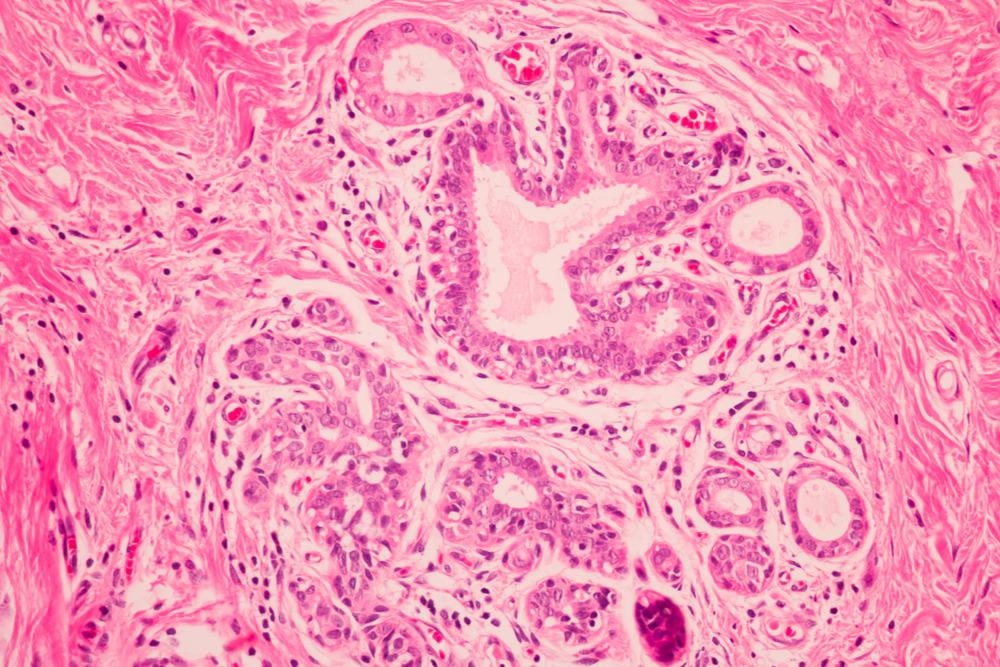
Due to the wide variation in morphology of breast cancer tumors, there are many different categories. They are categorized based on morphology as well as genomic and proteomic differences. The establishment of these differences helps with diagnosis and prognosis, ensuring the patient gets the treatment most suited to their specific form of cancer.
The two main categories are in situ and invasive carcinoma. In situ ductal and lobular carcinomas are separated by differences in cell type and function as well as differences in growth. Ductal carcinoma is further differentiated into subtypes by the tumor structure.
Invasive carcinomas are defined by their tumor structure, which can be medullary, tubular, or papillary, and their secretion which are either mucinous or colloid. Invasive ductal carcinoma is the most common form of breast cancer in the cancer genome atlas (CGA) and it accounts for between 70% and 80% of all invasive breast cancer tumors.
Screening Processes
Mammography detects between 2 and 8 malignant tumors per 1,000 scans. The three leading organizations that produce evidence-based guidelines for breast cancer screening and testing, the US Preventative Services Task Force (USPSTF), the American Cancer Society (ACS) and the American college of Radiology (ACR), all recommend that women aged between 50 and 74 undergo regular screening.
Mammography is the scanning of breasts to detect breast cancer using low-energy X-rays. Digital breast tomosynthesis (DBT), contrast-enhanced spectral mammography (CESM), magnetic resonance imaging (MRI) and ultrasound are all subdivisions of mammography used for the early detection of breast carcinomas.
DBT is a digital technique in which multiple low-dose X-ray images are taken across the breast. These are acquired after an iodine-based contrast media is injected into the desired site. The resulting image reduces false positives due to overlapping or aggregation of breast tissue. This technique has a 98% sensitivity although this is paired with a relatively low specificity of 58%.
CESM has a similar specificity and sensitivity to DBT and also requires the injection of iodine-based contrast media to image the desired tissue. This is due to the increased blood vessel proliferation around tumors being enhanced more readily than the surrounding tissue when a contrast media is injected into the bloodstream.
Breast MRI is one of the most efficient screening techniques, boasting a sensitivity of 90% or higher. The only other technique with a sensitivity comparable to it is positron emission mammography (PEM) although this is still in its experimental phase. It has a sensitivity of between 90 and 96% when interpreted by experienced readers although there are still doubts surrounding its ability to detect low-grade carcinomas.
Ultrasound is usually the first technique used to detect a malignancy and has been in use since the 1980s. Although it is effective at detecting breast cancers in conjunction with other mammography techniques, it does increase the need for callbacks and biopsies.
Breast cancer diagnosis. Image Credit: Komsan Loonprom/Shutterstock.com
Estrogen and Progesterone Receptors
As previously stated, breast carcinomas are classified based on their morphological, genomic, and proteomic differences. They are also classified based on the presence or absence of receptors, specifically estrogen receptors (ER) and progesterone receptors (PR).
Malignant tumors are subdivided into five categories based on their receptor expression and the presence of the mutated Her2 gene. Tumors possessing the ER are more commonly found than those that do not and generally tend to be smaller and lower grade than their counterparts. These ER-positive tumors are divided into two groups, Luminal A and Luminal B.
ER-negative tumors are divided into three distinct subtypes. The first of these types is defined by an increased expression of Her2 and its related genes. This group is known as the Her2 subtype. The second of these subtypes, the basal-like subtype, is characterized by increased expression of genes that would normally be associated with myoepithelial cells, found in the glandular epithelium, or basal cells, an epithelial stem cell.
The third subtype of ER-negative tumors does not have a defined gene expression profile and so is called the normal type subtype. It can express a variety of profiles and is not well defined.
There are some breast cancer tumors, triple-negative breast cancers (TNBC), that have no ER, PR or Her2 expression. They account for around 15% of all breast cancers and are more commonly diagnosed in younger women.
The Future of Breast Cancer Screening
The rise in breast cancer cases is a definite cause for concern but the wide variety of screening techniques and the new processes being developed offer hope for future cases. The large amounts of research being performed in the field also promise to improve screening processes and treatment courses.
References
- Mueller, C., Haymond, A., Davis, J. B., Williams, A., & Espina, V. (2018). Protein biomarkers for subtyping breast cancer and implications for future research. Expert review of proteomics, 15(2), 131–152. https://doi.org/10.1080/14789450.2018.1421071
- Niell, B. L., Freer, P. E., Weinfurtner, R. J., Arleo, E. K., & Drukteinis, J. S. (2017). Screening for Breast Cancer. Radiologic clinics of North America, 55(6), 1145–1162. https://doi.org/10.1016/j.rcl.2017.06.004
- Tao, Z., Shi, A., Lu, C., Song, T., Zhang, Z., & Zhao, J. (2015). Breast Cancer: Epidemiology and Etiology. Cell biochemistry and biophysics, 72(2), 333–338. https://doi.org/10.1007/s12013-014-0459-6
Further Reading
Last Updated: Mar 8, 2022