Interest in the microbiome of the reproductive tract has been growing over recent years. Studies of vaginal and placental microbiomes have shown associations between these microbiomes and obstetric outcomes and it is plausible that the uterine microbiome is also associated with these outcomes.
Since infection is a major cause of preterm birth, many studies over the last ten years have focused on identifying microorganisms residing in the uterus and recording any association with pregnancy outcome.
Current knowledge about the uterine microbiome has been greatly enhanced by the availability of molecular techniques in the field of microbiology, which has led to the discovery of various bacterial taxa that had not previously been described.
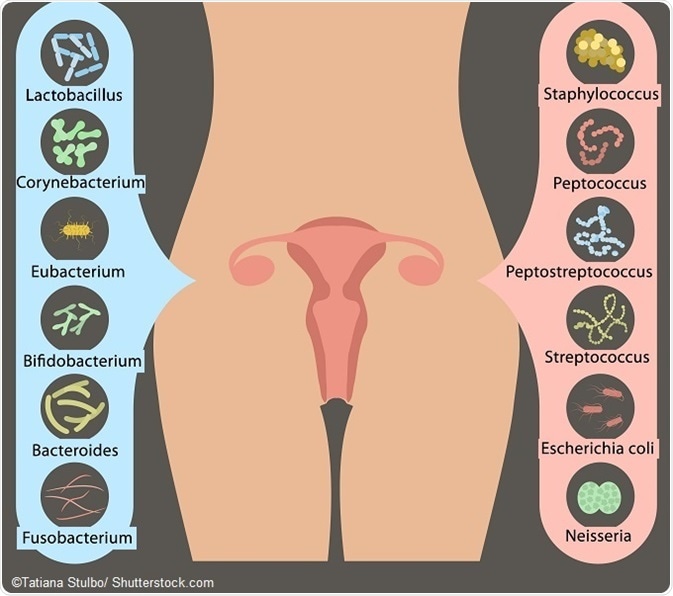
The bacteria present in the uterine cavity that so far seem to be the most strongly linked to negative outcomes in pregnancy are Ureaplasma sp. and Fusobacterium sp. Viruses are also present in the uterus, but they only seem to be significant contributors to preterm birth when they are present in combination with bacterial infection. Currently, researchers’ understanding of fungi colonizing the uterus is restricted to Candida species and further research is needed in this area.
The main pathway by which microbes have been thought to colonize the uterus is vertical ascension from the vagina, but research is beginning to suggest that microbes reach the uterus after they move from the mother’s mouth into the bloodstream when she cleans her teeth, for example. Some murine models have shown evidence of this route of microbial transfer, but further studies are needed to clarify this.
The uterine microbiome composition has also been explored as a contributory factor in the development of endometrial cancer. In a 2016 study, Nicholas Chia (Department of surgery, Mayo Clinic) and colleagues analyzed samples taken from the female reproductive tract (the vagina, cervix, ovaries and fallopian tubes) of patients who had endometrial cancer or hyperplasia and compared them with samples taken from patients with benign conditions of the uterus.
As reported in Genome Medicine, high throughput next generation DNA sequencing was used to identify the microbiota present, which showed that several taxa were significantly more abundant in the patients with endometrial cancer and hyperplasia compared with the patients who had benign conditions.
In particular, the presence of A. vaginae and Porphyromonas species, together with a high vaginal pH was significantly associated with the presence of endometrial cancer. The researchers say these microbes have previously been shown to be associated with other pathologies and that their results suggest a role of the microbiome in the cause and progression of this cancer that requires further research.
Further Reading
Last Updated: Feb 26, 2019