Jan 24 2005
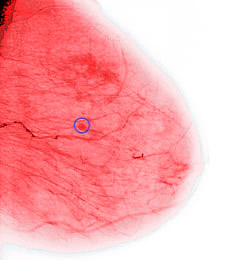 Annual mammograms and doctor visits are the best follow-up strategy for women who have been treated for early stage breast cancer, according to a new review of recent research.
Annual mammograms and doctor visits are the best follow-up strategy for women who have been treated for early stage breast cancer, according to a new review of recent research.
The report suggests that more intensive lab tests like liver scans and molecular tumor markers do not improve the chances of detecting a recurrence of cancer or increase survival rates among former breast cancer patients.
The finding is at odds with the usual treatment for breast cancer patients, according to Dr. Roldano Fossati of the Mario Negri Institute in Italy and colleagues.
Fossati says “intensive follow-up is quite common in clinical practice and represents a significant workload for radiotherapy, surgical and oncologic departments.”
The review appears in the January issue of The Cochrane Library, a publication of The Cochrane Collaboration, an international organization that evaluates medical research. Systematic reviews draw evidence-based conclusions about medical practice after considering both the content and quality of existing medical trials on a topic.
The new analysis is an update of a 20-year-old Cochrane report on the topic. The current review includes four randomized controlled trial studies of 3,055 patients that compare different types of breast cancer follow-up care.
After analyzing data from two of the studies, the researchers found no significant difference in terms of survival, detection of new cancers or quality of life between a group of women who got regular physical exams and annual mammograms and a group who underwent a more extensive battery of laboratory tests that included liver scans, molecular tumor markers, chest x-rays and blood and liver function tests.
Another study included in the review found that follow-up care by hospital-based specialists was not significantly different from that offered by general practitioners in terms of improvements in the patient’s quality of life or speed in detecting new cancers. However, patients were more likely to be satisfied with care by their general practitioner.
Despite studies indicating that routine physical exams are effective follow-up care, the National Cancer Institute’s treatment recommendations to health professionals notes that “the appropriateness of screening tests after the completion of primary treatment [for breast cancer] remains controversial.”
Although evidence favoring less intensive follow-up care began to appear in the late 1990s, “women still seemed to prefer a frequent schedule of tests in order to be reassured about their health status,” Fossati says.
“It would be worthwhile to evaluate whether a good strategy of sharing information between the doctor and the patient would help women to be equally reassured when a less intensive follow-up is offered,” he adds.
Fossati and colleagues acknowledge that the two main studies in their analysis were begun in the late 1980s, which may influence the review’s findings.
“One must consider that now, more than a decade later, knowledge, technology and treatment for breast cancer have improved, which may justify new randomized controlled trials,” Fossati says.