Feb 20 2005
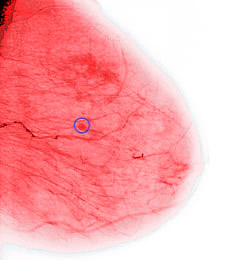 Researchers have discovered a genetic signature that can identify breast cancer patients at high risk of distant recurrence, reporting their results in this week’s issue of The Lancet.
Researchers have discovered a genetic signature that can identify breast cancer patients at high risk of distant recurrence, reporting their results in this week’s issue of The Lancet.
Currently, no reliable diagnostic tools exist to predict which breast cancer patients are most likely to relapse. Around 60-70% of women with lymph-node negative breast cancer are cured by local surgery and radiotherapy but guidelines recommend that 85–90% of these patients receive additional chemotherapy. The ability to identify patients who have a favourable prognosis could allow clinicians to avoid unnecessary treatment or choose less aggressive therapies for patients.
John Foekens and colleagues (Erasmus MC Rotterdam, Netherlands) and colleagues, looked at patterns of gene expressions in 286 tumour samples from patients with lymph-node negative breast cancer who had not received hormone or chemotherapy after their initial treatment. The sample group consisted of 209 patients, from all age groups and tumour sizes, including women who had oestrogen receptor positive and negative breast cancer. Patients were followed up for an average of 8 years and 93 (33%) were found to have cancer that had spread to another part of their body. The investigators analysed 115 of the tumours for a selection of markers and found a 76-gene signature that could predict disease relapse.
They independently tested the gene signature on 171 lymph-node negative patients and found it could accurately predict patients who developed distant recurrence within five years (93% sensitivity) but was less accurate at predicting patients whose disease did not return within 5 years (48% specificity).
Dr Foekens concludes: “Since only 30-40% of untreated lymph-node negative patients develop tumour recurrence, our prognostic signature could provide a powerful tool to identify those patients at low risk preventing overtreatment in substantial numbers of patients. If confirmed in further studies, the recommendation of additional hormone or chemotherapy in patients with lymph-node negative breast cancer could be guided by this prognostic signature.”
In an accompanying commentary Tor-Kristian Jenssen (PubGene AS, Vinderen, Norway) and Eivind Hovig (Norwegian Radium Hospital, Montebello, Norway) state that several large scale breast cancer studies have identified signature gene lists that could potentially predict clinical outcome but when comparing these there is virtually complete lack of agreement in the genes included.
Dr Jenssen comments: “Faced with alternative gene signatures for very similar prediction problems, we are left with the obvious questions of which to trust and why they differ. Although Wang and colleagues present the largest study of this type of data, it may still be too small to provide a final selection of genes for signature inclusion. Thus the signature is there, but it is still necessary to read the fine print.”