May 26 2009
Stem cells that respond after a severe injury in the lungs of mice may be a source of rapidly dividing cells that lead to lung cancer, according to a team of American and British researchers.
"There are chemically resistant, local-tissue stem cells in the lung that only activate after severe injury," said Barry R. Stripp, Ph.D., professor of medicine and cell biology at Duke University Medical Center. "Cigarette smoke contains a host of toxic chemicals, and smoking is one factor that we anticipate would stimulate these stem cells. Our findings demonstrate that, with severe injury, the resulting repair response leads to large numbers of proliferating cells that are derived from these rare stem cells."
Stripp said this finding could be related to the increased incidence of lung cancer in people with chronic disease states, in particular among cigarette smokers.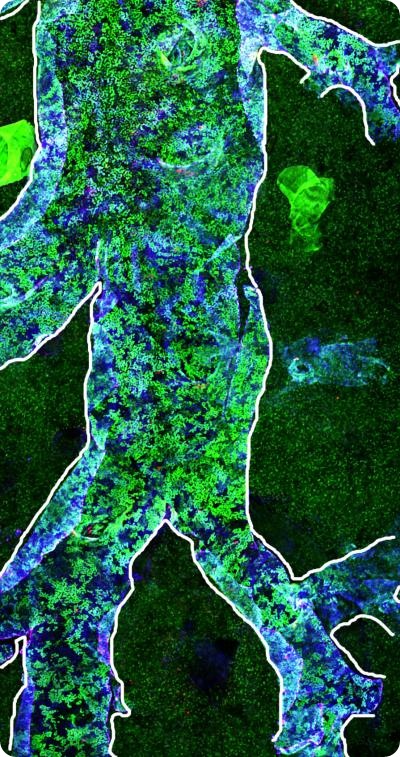
The findings were published in the advance online edition of the Proceedings of the National Academy of Sciences during the week of May 25.
"On the positive side, I think that it might be possible to improve lung function in the context of disease if we could understand which pathways regulate lung stem cell activation and then target these pharmacologically," said lead author Adam Giangreco, Ph.D., from Cancer Research UK's Cambridge Research Institute. "In terms of lung cancer susceptibility, however, our observation that stem cell activation leads to clonal expansion after injury could, in the context of additional mutations, promote the development of cancerous or precancerous lesions from activated stem cells."
The scientists used a chimeric mouse model, part wild-type and part with green fluorescent protein-tagged cells (GFP), so that the behavior of different populations of duplicating lung cells could be evaluated with high-resolution imaging methods. By understanding the extent to which GFP-positive and GFP-negative cells were mixed, the investigators were able to show that the abundant population of progenitor cells that normally maintain the epithelial layer in the lung could be rapidly wiped out with a strong chemical, naphthalene. Then the rare proliferative cells became active and grew into large patches.
The researchers at Duke and Cancer Research UK used a unique whole-lung imaging method to examine and identify the location of stem cells in the lung tissue of mice, and determine the role they play in both healthy and damaged mouse lungs.
They found that, while the stem cells don't appear to be involved in the normal maintenance of healthy or moderately injured lungs, they do play a vital role in repairing severely damaged lungs.
Even though this repair mechanism is important for restoring lung function, it can come at a price. An acquired mutation in that rare cell or its descendants leads to clonal patches of many identical cells. Secondary mutations in any one of these cells may provide the signals needed for unregulated cell growth and tumor progression.
"This work provides a plausible mechanism to account for this type of event that we previously didn't have," Stripp said.
The study was supported by grant funding from the National Institutes of Health, Cancer Research UK, the University of Cambridge and Hutchison Whampoa. 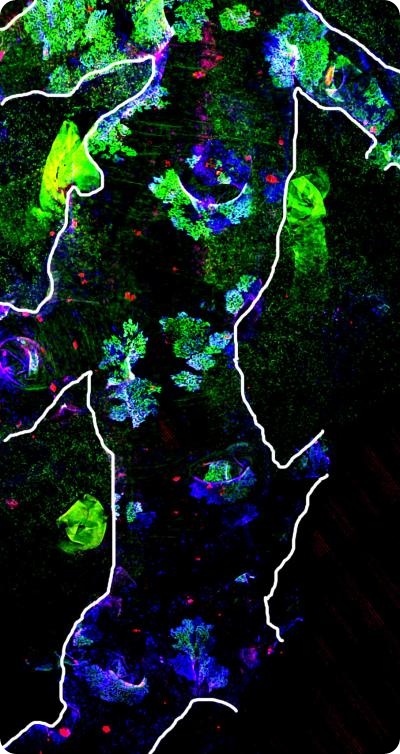
Other authors include Joshua Snyder from the Duke Department of Medicine; Esther Arwet and Fiona Watt of Cancer Research UK's Cambridge Research Institute; and Ian Rosewell with Cancer Research UK at the London Research Institute in South Mimms. Dr. Watt is also with the Wellcome Trust Centre for Stem Cell Research at Cambridge University.