Overactive bladder symptom complex is a symptom complex, the pivotal symptom of which is urgency, which is a compelling desire to pass urine, which is difficult to defer.
If you get urgency this will lead onto frequency, which is an increased frequency of urine production which can occur in the daytime, or at night-time, when it is known as Nocturia.
It also leads to reduced volume voided, and if patients get urgency, particularly female patients, as in a third of females with overactive bladder, they can't make it to the toilet in time and they get incontinence, which is known as urgency incontinence.
Obviously if patients are getting symptoms of this nature, they need to see their doctor. In that context the most appropriate investigation first off, is for them to fill out a bladder diary to record the frequency of voids, passing urine, and what other symptoms they are experiencing.
If necessary, their doctor will either start them on therapy, give them advice about lifestyle, and/or refer them to a specialist.
What treatments are currently available for overactive bladder symptom complex?
It's very important for the investigations to be carried out, mainly a bladder diary and assessment of fluid intake. Lifestyle advice may be necessary in some patients.
It's also important to exclude other pathology, such as increased urine production at night-time, so called Nocturnal Polyuria where more than a third of the 24-hour urine production is produced at night-time. And that includes the voids during the night, which wake somebody from sleep, sleep disturbing voiding, which is the definition of Nocturia. Going twice or more times at night is counted as being potentially clinically significant. In making this calculation of Nocturnal Polyuria, one needs not only to add in the volumes produced at night-time, when somebody has woken from sleep, but also the first void of the morning when somebody is getting up.
Having made the diagnosis, and excluded these other problems such as increased fluid intake, increased urine production at night-time, which can be due to other physiological conditions such as diabetes, heart failure, or fluid retention, then patients can be considered for treatment with agents which reduce bladder over activity which act on the bladder. These are either known as anticholinergics, or there is a beta-3 agonist, which has recently been introduced.

L-R: Professor Chris Chapple, a leading urological surgeon and scientific lead of the Training Urology Scientists to develop Treatments project with two of the project’s young researchers Sabìniano Roman, Martin Slovak and project manager Michelle Battye with the new portable electrical stimulator.
A multi-million European Union funded project looking to find new treatments for bladder problems was announced around 2 years ago. Why is it necessary to find new treatments for overactive bladder syndrome?
The reason for a research program, which has been lead from Sheffield, looking at this area, is because this is a condition which is extremely important affecting up to 10% of the population at any one time.
The existing therapies need to be improved upon because they do have side effects in some patients, particularly the anticholinergics. And these side effects can be so troublesome in patients that they lead to people not being able to tolerate them.
In addition, obviously, we need to advance our knowledge in this area to understand what causes the overactive bladder symptom complex so we can find better ways of treating this condition. This is particularly important because we have an aging population and this condition increases with age, and so it's inevitably going to become more prevalent in the population, and more of a problem because of the impact it has on activities: daily living, lifestyle, and indeed on quality of life therefore.
What hurdles do you expect researchers will face when trying to develop new treatments for overactive bladder syndrome?
The principal hurdle is firstly to identify the exact underlying cause of the symptom complex. As I've mentioned already, it's not just a simple diagnosis based on symptoms because one has to consider that the bladder is an unreliable witness. Because symptoms are not disease-specific, the identification of symptoms will vary upon the way in which they are reported, and the way they are interpreted by a clinician. At the end of the day, even having made a symptom complex diagnosis, it's important to understand the underlying pathophysiology both in terms of bladder dysfunction, as well as other dysfunctions, which occur in the body, which can be affecting the production of urine and its storage by the bladder.
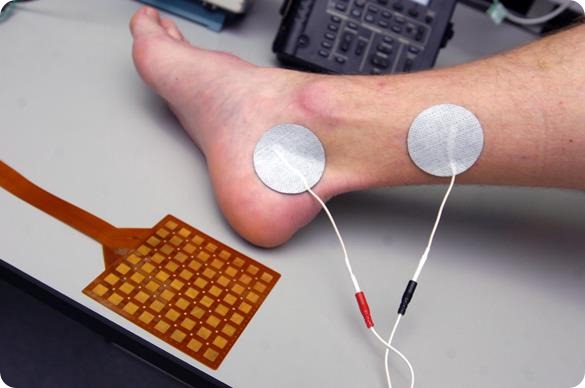
The new electrical stimulation therapy device.
Please can you tell us about the new treatment Martin Slovak, a biomedical engineering graduate from the Brno University of Technology in the Czech Republic, is working on?
There are various ways of treating overactive bladder symptom complex. The first and important way of treating it is to identify any underlying causes with a bladder diary. And with this in mind, one can then progress on either to drug therapy, which in recent years has been the mainstay of therapy, but also there is increasing evidence that it is possible to use other non-drug therapy related approaches such as electrical stimulation.
Martin Slovak is working on a new treatment which is based on existing therapy, but which may prove to be more cost effective and easier for patients to use, as it's non-invasive and does not involve inserting needles into the patient. But by using surface electrical stimulation may be effective, and therefore provide a useful alternative to existing therapy in this area.

Martin with the new electrical stimulation therapy device.
How long would you expect a new treatment like this to take to develop?
It's to be expected that a new therapy such as this will take 18 months to 2 years to go through validation and careful assessment in a randomised fashion against a placebo arm to identify that there is a significant treatment effect size, which can be achieved with this new therapy.
What impact do you think a new treatment for overactive bladder syndrome would have on the quality of life of patients?
Overactive bladder symptom complex is very intrusive in terms of quality of life because of the disruption it has both day and night on people's activities. Waking people at night, which is Nocturia, or sleep disturbed voiding, has significant consequences as people become very tired, and has a knock on effect for the next day if they are tired.
Also it disrupts quality of life. In the daytime, getting a compelling desire to pass urine when somebody is doing something, for instance in the car on the motorway, or going out shopping, or socialising, can be very disruptive and embarrassing. In female patients, up to a third suffer urgency incontinence. Incontinence is an extremely depressing symptom, which obviously has enormous consequences in terms of social isolation.
So there is no doubt that any new therapies which will be effective in improving the symptoms of overactive bladder symptom complex, whether that's frequency, Nocturia, urgency, or urgency incontinence, will have a significant impact on quality of life.

The new electrical stimulation therapy device.
Would an at-home portable electronic device be an economically efficient treatment?
Yes if it's provided through the NHS, as an NHS development under the NHS supported program Devices for Dignity, it would be very cost effective as the capital cost of this treatment would be no more than two months’ supply of drug therapy.
How exactly is this project being funded?
The project is being funded by the European Commission’s 7th Framework Programme for Research and Technological Development.
Where can readers find more information?
At this stage the therapy is under development so there is no specific information available about it although people who are interested could always contact the Bladder and Bowel Foundation for assessment of patients and their treatment: http://www.bladderandbowelfoundation.org/
They can find more information on the TRUST at: https://trust-project.eu/
About Professor Chris Chapple
 Professor Christopher Chapple is a Consultant Urological Surgeon at Sheffield Teaching Hospitals and Visiting Professor at Sheffield Hallam University. He has a particular interest in functional reconstruction of the lower urinary tract and the underlying pharmacological control mechanisms and provides a tertiary service in lower urinary tract reconstructive surgery. He trained at the Middlesex Hospital where he subsequently completed his doctorate thesis, and continued there and at the Institute of Urology in London for his sub-specialist training.
Professor Christopher Chapple is a Consultant Urological Surgeon at Sheffield Teaching Hospitals and Visiting Professor at Sheffield Hallam University. He has a particular interest in functional reconstruction of the lower urinary tract and the underlying pharmacological control mechanisms and provides a tertiary service in lower urinary tract reconstructive surgery. He trained at the Middlesex Hospital where he subsequently completed his doctorate thesis, and continued there and at the Institute of Urology in London for his sub-specialist training.
He is Chairman of the International Relations Committee at the European Association of Urology, having previously been the Adjunct Secretary General responsible for Education and Past Director of the European School of Urology. He is editor-in-chief of the journal Neurourology and Urodynamics and is on the editorial board of several journals such as the British Journal of Urology, European Urology, Surgery and Current Opinion in Urology. He is an active member of many international urological associations and societies including the British Association of Urological Surgeons, the European Association of Urology, the International Continence Society, the Association of Academic European Urologists and the American Association of Genitourinary Surgeons. He has chaired a number of guidelines initiatives including the NICE Guidelines Development Group on male lower urinary tract symptoms. He was awarded the St Peter’s medal by the British Association of Urological Surgeons in 2011. Professor Chapple has co-authored over 350 articles in peer-reviewed Journals and has written several books and a number of book chapters.