Generally speaking, reflux has been a major chronic issue for probably the last 40 or 50 years. When you look at the global population, depending on which country we're talking about, around 20% to 40% of individuals have reflux disease within their populations.
The stomach contains gastric juice (refluxate), which consists of acid, bile acid, and pepsin – the marker we're going to be describing in more detail – as well as, obviously, food. There are other things in the stomach such as mucus and bicarbonate but the really aggressive factors are the acid, bile acid and pepsin.
When we describe gastroesophageal reflux, we're really describing reflux into the lower part of the oesophagus which has more of the classical symptoms such as heartburn and regurgitation.
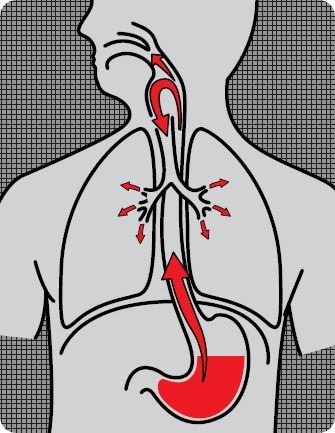
In the last 20 years, we have become aware of extra-oesophageal reflux which is reflux that goes way beyond the oesophagus, passing through the upper oesophageal sphincter and into the airways and the throat. There is also a risk of it passing into the lungs. This reflux has a different symptom profile characterized by symptoms such as hoarseness, sore throat, voice disorders, chronic cough and even asthma. It is estimated that probably between 20% and 30% of people have this type of reflux.
Some people will have both. When you look at the data, probably about 30% of people with reflux will have both the more classical symptoms as well as these extra-oesophageal symptoms. The other interesting fact about reflux disease is that the more classical symptoms, such as heartburn, normally manifest at night while a person is lying in the supine position. With extra-oesophageal reflux, however, the reflux can occur in more upright positions, so a person may have a reflux event when they are up and walking around.
Overall, we can estimate that 40% or maybe even 50% of the world's population and that includes from young babies to the older generation, will have some form of reflux at some time.
Also, it is a chronic condition. Some people may have daily reflux, some weekly, some monthly, and some may only have an occurrence a few times a year, but it is still a chronic condition.
How are reflux diseases currently diagnosed?
When a patient is suspected of having reflux disease, in the first instance, they go to their primary care physician, or if they're in the UK, their GP. They describe their symptoms and assessment is based very much on patient history.
However, to actually show whether they do have reflux, two things often happen. Firstly, in the UK, and many countries, current guidelines often recommend a course of proton pump inhibitors (PPIs) without a definitive diagnostic procedure; in many cases this is actually not a good idea.
The reason this should be avoided is because people should only really be taking PPIs if they have a confirmed acid reflux diagnosis, not just because reflux is suspected. Using PPIs for more than four weeks can make it quite hard to come off the drug once you're on it.
The second thing that happens is that patients are sent for one or more of a series of very invasive diagnostic tests; the main one being endoscopy. In this scenario the patient would be referred to secondary care and it's highly likely that they would have an endoscopy involving a tube being orally inserted and passing into the oesophagus.
Another invasive test is 24-hour ambulatory dual-probe pH monitoring, which again involves a tube being nasally inserted, but with this test, the tube passes right down into the oesophagus where it sits just above the stomach for 24 hours. Also, it is taped to your nose and face. It’s a very common test used to look for pH changes over a 24-hour period. In other words, it measures reflux by looking at changes in acidity inside the oesophagus due to reflux.
Then there's a newer test which builds on the one just described, called the 24-hour pH impedance test. This usually involves dual pH probes, one to measure the pH in your oesophagus and another to measure the pH in your airway. However, what it is also capable of doing is measuring the height of the gastric refluxate, so it can actually see if the reflux is coming up from the stomach to just the bottom part of your oesophagus or whether it’s coming right up into your airways.
In addition, there is something called high-resolution manometry, which again involves using a tube to examine reflux and also swallowing behaviour. This is also invasive.
There's also a wireless pH monitoring system called Bravo and something called Restech (minimally invasive), which is a pharyngeal pH test. However, all of these are invasive tests and, obviously, a lot of patients are uncomfortable with having these sorts of tests and may refuse to have them.
Other invasive tests are carried out by the ear nose and throat (ENT) specialists, where a lot of patients with reflux symptoms are seen. In this case, fiber optic transnasal laryngoscopy will be performed in which a tube with a little camera attached is placed up the nose so that the voice box and vocal chords can be examined. Although this procedure is not as invasive as some others, it is still unpleasant for the patient.
What prompted RDBiomed to create a non-invasive reflux test?
I've been working on reflux disease since 1981. In those days, histamine receptor antagonists such as cimetidine and ranitidine had been launched and were the first acid suppression agents on the market. The proton pump inhibitors weren't even launched at that time, but a product called Gaviscon was available which I’d been involved with during the early stages of development.
We were trying to understand what reflux was and we all believed that acid was the cause of all the problems. It probably wasn’t until the beginning of the '90s that it occurred to us that the pepsin present in the gastric refluxate might be one of the causal factors of reflux disease symptoms and I did a lot of basic research into pepsin.
Then, in 1997, we started a pepsin reflux clinical development program to have a look at pepsin in more detail in reflux. In 2004, we started working on a development program for Peptest, our present pepsin diagnostic, because it became clear that we could actually use pepsin as a marker of reflux. Pepsin is only found in the stomach, so, if we find it outside the stomach such as in the oesophagus, the throat, the mouth, the lungs, then we know it has been refluxed.
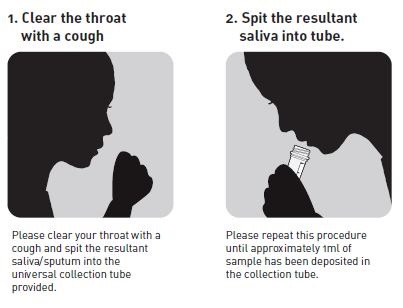
We started using pepsin as a marker of reflux and began to realise the potential it has as a non-invasive test. We ask patients to provide a saliva/sputum sample that they just spit into a collection tube for us to analyse, so it's completely non-invasive. We’ve tested thousands of patients in this way and not one patient has ever refused to provide a sample in this way.
We realised quite early on that a major issue with the traditional invasive diagnostic tests was compliance. This was especially true among the elderly and child populations, who weren't really comfortable with the process of having tubes inserted for long periods of time.
Another drawback with the traditional tests is that although you can tell patients who have the tube in place for 24 hours, to carry on with life as usual, and eat normally, sleep normally, etc., there they are with a tube taped to their nose and going down all the way to their stomach, so actually, they don't eat normally and they don't behave normally.
This can often affect the amount of reflux a patient experiences and can lead to the risk of getting negative results back because patients are not behaving in the way they would if they didn't have the tube in place; thus in some cases the results are possibly not specific or sensitive for reflux disease.
Therefore, we decided to create a non-invasive test that measures pepsin as a marker of reflux in saliva/sputum and that led us onto developing the Lateral Flow Device that we have now. It's very similar to a pregnancy test, really. You actually take the saliva sample and you prepare it in a certain way and add a small amount to the well of the Lateral Flow Device. If pepsin is present in the sample the device will produce a positive result confirming the diagnosis of reflux.
As described earlier compliance is an issue with invasive tests, as well as sensitivity and one other big issue, depending on the country you're performing the test in, is cost, the cost can be very high for invasive diagnostic tests.
In the UK, for example, these invasive tests cost hundreds of pounds. Also, although the waiting list is shorter than it used to be, it can still take quite a long time for people to receive diagnostic test because they still have to be put on a waiting list to receive an appointment, which can take several months. It is important to consider that endoscopy clinics are a valuable resource for the detection of many cancers so any way that waiting times can be reduced by removing unnecessary procedures from the schedule is vital for the NHS.
Is that the reason why GPs often put patients on the proton pump inhibitors you mentioned?
Yes. What they often do is to put the patient on to a proton pump inhibitor until they can get a secondary test done. And so, the patient is put on a proton pump inhibitor even though they haven't been properly diagnosed for reflux disease, while they wait to see if they are positive or not and, obviously, a lot of those tests will come back negative. If they do an endoscopy, probably 50% won't actually show anything.
Also, of the patients who have been on acid suppression therapy for a few months, if and when they do come off them, they get something called hyperacidity. Because the inhibitors prevent acid, they can cause acid rebound so that patients can potentially end up with more acid than they had in the first place. So, patients who didn't actually have reflux in the first place, suddenly develop it because they've got an excess of acid.
Please can you explain how PeptestTM works?
Peptest measures the presence of pepsin in a clinical sample, usually of saliva or sputum. All the patient is asked to do is to spit a very small sample, a 1 ml sample is fine, into a tube that contains a very low concentration of citric acid – it has 0.01 M citric acid in the collection tube. This is to keep the pepsin stable at the right acidity because it is a very aggressive enzyme that will otherwise destroy itself before we have a chance to analyse it. The instructions below illustrate how simple the sample collection process is.
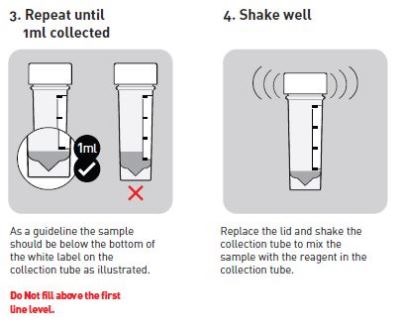
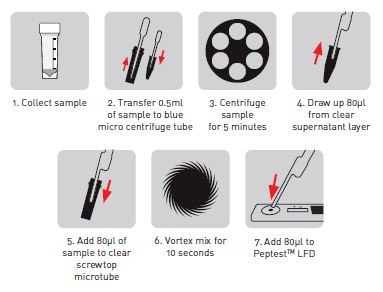
We take half a ml of the clinical sample from the tube and we centrifuge it at 4000 rpm, so it's a very, low centrifugation. We centrifuge it for five minutes and this gives us what we call a supernatant, a clear layer, and a pellet of debris at the bottom of the centrifuge tube.
We take out 80 microliters of the clear supernatant layer and add it to 240 microliters of migration buffer, (a special buffer of a certain pH which is used in Lateral Flow Device technology to help samples flow through the system).We then mix that for 10 seconds remove 80 microliters of the mixture, which now contains our clinical sample plus migration buffer and add it to the well of the Lateral Flow Device – Peptest
We have developed Peptest with two unique monoclonal pepsin antibodies which are owned by us. We’ve developed them and so we are the only people in the world that have them. One of the antibodies we use to detect pepsin and the other is used to capture pepsin.
The Lateral Flow Device is designed in such a way that, underneath the sample well where you add the clinical sample, sits the antibody that detects pepsin – this means the antibody attaches itself to the pepsin within the sample. Also attached to the antibody are blue latex beads that effectively label the pepsin.
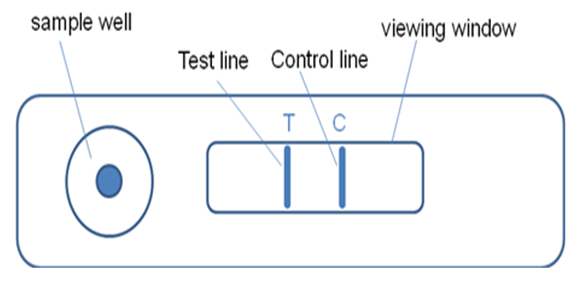
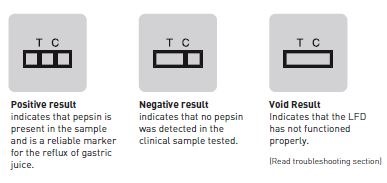
The sample will then be carried through the device by the migration buffer and, if pepsin is present, the detection antibody will carry it to the capture antibody, which is impregnated at the 'T' line or test line of the device. The pepsin and blue latex beads will be held at the T line by the capture antibody and cause a blue line to appear indicating that pepsin is present. The more pepsin that is present the more blue latex will be captured and thus the more intense the blue line.
The excess blue latex will pass on to a control line, where a secondary antibody is used to demonstrate that the lateral flow system has worked. So, if we ever got a Lateral Flow Device where the control line didn't light up blue, then the device hasn't worked and we would repeat the test. But in all honesty, in the thousands we've tested, that's never happened because it’s designed not to happen.
If you end up with a 'T' line that is blue as well as a control line that is blue, you know that pepsin is present in the sample.
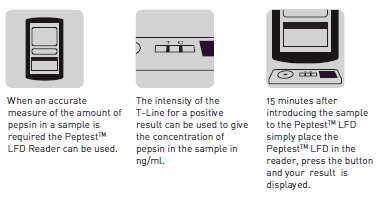
We've also developed what we call a Lateral Flow Device reader so that we can read off the intensity of the blue lines in nanograms per ml of pepsin. This means a report can be generated, whether it be for doctors or patients, that will provide some idea of the level of pepsin present in the sample
Some doctors only want to know whether pepsin is present or not, but others, especially the ones in research, want to know how much because they may want to put the patient onto a treatment regime, and maybe retest them at a later date to see if levels have reduced. Also, if they are going to perform anti -reflux surgery, it means they will be able to compare a pre- and post-surgical reading to see if the pepsin levels have reduced or disappeared.
Does PeptestTM differentiate between the different types of reflux or are further tests required on the identification of the presence of pepsin?
What it tells you is that the patient has pepsin present and so it indicates that the patient does reflux. What tells you the type of reflux they have is their symptom profile. Some will present with heartburn and regurgitation and some will present with the more airway type symptoms such as chronic cough, asthma or hoarseness, which is what really differentiates the type of reflux. The Peptest will tell you that reflux is present.
But there is another interesting factor that might help answer your question. Acid, which is suggested to cause reflux disease symptoms, is actually only destructive up to pH 3 or 4. Whereas, we know that pepsin is not denatured until you get to pH 6.5 or 7.0. So, while acid will have disappeared, pepsin may still be present and potentially causing damage. Therefore a person could have acid reflux, weak- acid or non-acid reflux and pepsin is a very good indicator of all different types of reflux because it's not deactivated at low pH.
So, to summarise, acid reflux normally describes reflux of up to pH 4, weak acid reflux a pH of 4 to 7, and non-acid reflux at a pH of above 7. That is very important to know because there are a lot of patients on proton pump inhibitors who still have symptoms and the reason is because the proton pump inhibitors were designed to treat acid reflux, which is mainly the reflux in the lower part of the oesophagus but they were not designed to treat the airway type reflux, so a different treatment regime is needed.
How accurate is PeptestTM compared to current diagnostic procedures?
There are several clinical studies going on at the moment to actually demonstrate its accuracy. A recent study that was presented at United European Gastroenterology Week (UEGW) in Berlin, described Peptest as having a sensitivity of 95% and a specificity of 89%.
You'll find that those figures are comparable, if not higher, than any of the other sensitivities and specificities for the invasive tests. It has been suggested that Peptest may become the gold standard for test for diagnosing reflux disease because it's non-invasive, it's cheap, and it's highly specific, whereas the others are invasive, expensive and less specific.
Is Peptest economically efficient?
We've been working with various groups and most of this work is actually being done in the United Kingdom, which helps quite a lot. We're in the process of talking to the Clinical Commissioning Groups and are putting case studies together to demonstrate the benefits of Peptest and how Peptest can be used. There are various models demonstrating the sort of savings Peptest would bring to the NHS, if introduced.
We are also working with the Academic Health Science Network (AHSN), which has been set up by the government in the last few months across all regions in England. The principle role of the AHSN is to look at ways of making the National Health Service more efficient, to introduce innovations, and to lower the cost of patient care.
We have done some modelling and we have looked at a significant cohort of reflux patients who we know don't respond to proton pump inhibitors who would go on to have endoscopy. If we introduced the Peptest in place of endoscopy in just the Yorkshire and Humber region, the model suggests we could save the NHS around £2.5M, per annum. If we introduced it across NHS England, we could potentially save the NHS in the region of £21.5M per annum, which is quite exciting.
The figures quoted above are for a small proportion of patients that could benefit from using Peptest. If we work on the basis that all clinicians or at least some clinicians anyway, would like to have Peptest introduced into primary care and have it as a first-line approach and used as a screening tool, then it is estimated that the savings could be an order of magnitude higher.
So, there are some big figures and some big savings. However, to do that, you'd have to have a whole cultural change, because instead of using proton pump inhibitors as a first line treatment approach, before you even know if you're dealing with reflux, you'd have to do a Peptest.
What do you think the future holds for reflux disease diagnosis?
There are easier ways, quicker ways, cheaper ways and non-invasive ways to diagnose reflux. So it would mean that patients would be diagnosed much more quickly and would therefore get onto a treatment regime or a lifestyle regime much more quickly.
Also, there are patients who may present with symptoms they believe are due to reflux, but in actual fact they're not. A Peptest may be negative because they actually haven't got reflux, they've only got similar symptoms. You then know that those symptoms need to be looked at and treated in a different way.
For example, they may have allergies, they may have a food allergy and inflammation in the stomach, which has nothing to do with reflux and so needs to be treated in a different way.
So, the future of reflux disease is that we will be able to use Peptest to diagnose patients more quickly and more accurately than we are at the moment.
Also, the patient comfort and non-invasiveness of the procedure is important. We've been involved in a study looking at how patients perceive their reflux disease and how they perceive the diagnosis and the treatment they get.
A series of interviews were carried out with patients who first attended primary care, and then went right the way through secondary care and the procedures carried out and how long it took to get a diagnosis were discussed. It takes a long time, many months or years, as well as being very uncomfortable. So we know from these patients who were interviewed – and this was, again, done independently of us – would prefer to have a non-invasive quick test.
What are RD Biomed’s plans for the future?
Our plan for the future is to extend our work internationally. We have so far introduced Peptest in to 18 countries so we have started to export and go through all the regulatory procedures in certain countries.
The big target for us is the USA, where we need to get registration through the FDA. At the moment, we have MHRA registration and are CE marked, for UK and Europe but we're not into the USA yet. Our plans for the future are to establish Peptest within the NHS and to internationalize Peptest in a much more efficient way than we're doing at the moment.
Where can readers find more information?
About Peter Dettmar
 Professor Peter Dettmar is the former global Research and Development Director - Gastrointestinals for Reckitt Benckiser Healthcare (UK) Limited with extensive experience in running product development programs and clinical trials and over thirty years experience of the pharmaceutical and healthcare industries.
Professor Peter Dettmar is the former global Research and Development Director - Gastrointestinals for Reckitt Benckiser Healthcare (UK) Limited with extensive experience in running product development programs and clinical trials and over thirty years experience of the pharmaceutical and healthcare industries.
He has an Honorary Professorship with the School of Pharmaceutical Sciences University of Nottingham, UK and was Adjunct Professor and Director of Research at the Centre for Voice and Swallowing Disorders, Department of Otolaryngology, Wake Forest University Baptist Medical Centre, Winston-Salem, USA.
He has a PhD. in pharmacology from the University of Bradford, UK and is a named inventor on over 40 patents, has supervised more than 70 successful Ph.D. studentships and has authored or co-authored over 480 scientific and clinical publications.
He has a special interest in reflux disease, pepsin, mucosal protection, bioadhesion, H. pylori, nutrition, dietary fibres/functional foods, Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), polymers/biopolymers, cell biology and has established international research and clinical networks that are core to research in these areas.
He has organised national and international conferences and workshops including a series of meetings on reflux disease and symposia on human pepsin and gives numerous national and international lectures.
He has also established Technostics Limited and RD Biomed Limited two innovative healthcare and diagnostic companies based at Castle Hill Hospital in Cottingham East Yorkshire, UK.