What is autoimmune epilepsy, and how does it differ from other forms of epilepsy?
Epilepsy is a group of neurological disorders often characterized by seizures and cognitive impairment due to electrical disturbances in the brain.
While brain tumors, trauma or infection can cause epilepsy, the condition can be inherited genetically within families.
A growing body of literature demonstrates an autoimmune basis in the etiology of some forms of epilepsy.
A study published in the March 2014 edition of JAMA Neurology found that autoimmune disorders were associated with elevated risk of epilepsy, and that “patients with either condition should undergo surveillance for the other.”
Accurate diagnosis of the patient’s specific form of epileptic disorder is critical. Some forms of epilepsy may be treated with antiepileptic pharmacotherapy or surgical procedures, but the type and efficacy of treatment depends on the specific epileptic disorder, among other factors.
When and how was the condition discovered?
The link between autoimmune diseases and epilepsy without a recognized neurological cause has been documented for well over a decade.
However, the JAMA study published in March 2014 provides the largest known empirical evidence of the association between the two conditions.
Researchers analyzed claims data related to epilepsy and 12 autoimmune diseases from more than 2.5 million people.
The findings indicate the risk of epilepsy is almost four times higher for patients with an autoimmune disease, with 17.5 percent of epilepsy patients also having an autoimmune disease.
How common is this form of epilepsy?
Up to 2.3 million adults in the U.S. have epilepsy and nearly 150,000 develop the condition each year, according to estimates from the U.S. Centers for Disease Control and Prevention. Of these, as many as 10 percent may be categorized as autoimmune epilepsy.
Who is most at risk of autoimmune epilepsy?
The JAMA study is disturbing because it found a strong association between incidence of epilepsy and twelve autoimmune diseases, some of which are prevalent.
These twelve diseases are type 1 diabetes mellitus, psoriasis, rheumatoid arthritis, Graves' disease, Hashimoto's thyroiditis, Crohn's disease, ulcerative colitis, systemic lupus erythematosus, antiphospholipid syndrome, Sjögren syndrome, myasthenia gravis, and celiac disease.
Another disconcerting finding from the study was that while epilepsy can occur to patients of all ages, the risk is higher in children than adults.
How is autoimmune epilepsy currently diagnosed?
The cause of epilepsy is unknown in more than a third of individuals, and current diagnostic approaches can provide unclear results.
Physicians typically diagnose the type of epilepsy based on a comprehensive medical exam that includes assessing signs and symptoms and results of neuroimaging and electroencephalography (EEG) tests.
However, these tests, such as MRI, cerebrospinal fluid and brain biopsy, often provide unclear diagnostic information, and can be invasive and costly. Worse still, the results are often inconclusive.
In recent years, some diagnostic companies have begun to offer testing based on next-generation sequencing, which identifies variants associated with different forms of epilepsy.
This is a major advance because these assays can help pinpoint the genetic cause and use a blood sample, which is relatively less difficult and painful for the patient. However, these tests may provide a lot of information on variants that aren’t clinically meaningful, at least not for the individual patient.
Autoimmune epilepsy requires different diagnostic techniques. For this disorder, in addition to imaging exams like MRI and cerebrospinal fluid, molecular tests can identify particular autoimmune markers implicated in the condition through a blood test.
To identify autoimmune epilepsy, patients are also screened for a broad range of neural autoantibodies while MRI and cerebrospinal fluid testing may help identify inflammatory changes.
Please can you outline the new test Athena Diagnostics has developed for autoimmune epilepsy?
We have just released a multi-analyte panel to enable the physician to streamline the evaluation of a patient based on the presence of antibodies well correlated in the literature with autoimmune epilepsy.
It is the first clinically available multi-analyte test to identify five antibodies correlated with autoimmune epilepsy in the United States.
Athena Diagnostics Autoimmune Epilepsy Evaluation lab-developed test identifies antibodies directed against neuronal cell-surface antigens, such as NMDAR, VGKC-complex, LGI1 and CASPR2 as well as neuronal GAD65.
With this information, a physician may arrive at a reliable diagnosis more quickly, and initiate immunotherapy as well as traditional anticonvulsant therapy. We believe this test therefore reflects a significant diagnostic advance for autoimmune epilepsy.
What other epilepsy tests is Athena Diagnostics introducing?
The challenge of diagnosis by conventional methods is the reason Athena Diagnostics developed its suite of epilepsy tests based on next generation sequencing.
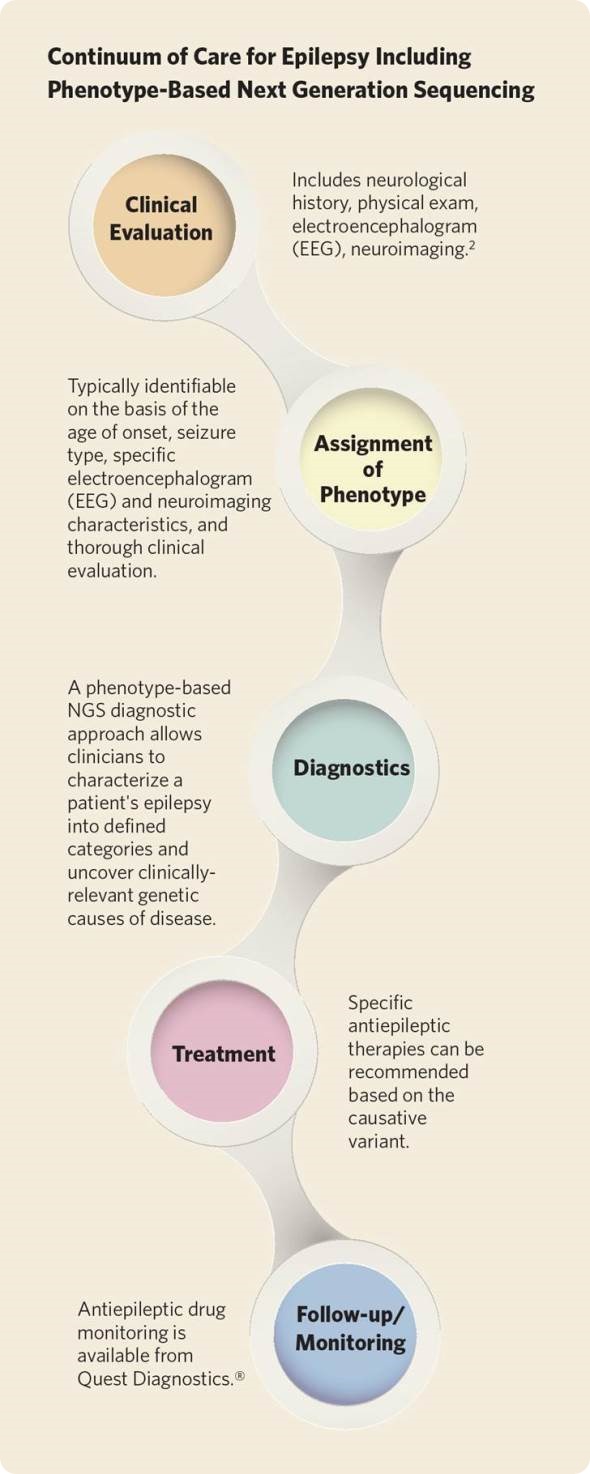
In addition to the autoimmune epilepsy test, we have introduced nine highly-targeted molecular sequencing test panels, according to epilepsy type, to aid the diagnosis of discrete forms of epilepsy ranging from generalized to syndromic.
The panels, called Epilepsy Advanced Sequencing Evaluations, are arranged by clinical phenotype and EEG test findings, with testing performed only on genes associated with a specific epilepsy type.
The advantage of this approach is that it helps the physician evaluate the patient’s test result within the larger context of her signs, symptoms and EEG test results. This differs from other NGS tests that provide a lot of data on molecular variants without a larger context in which to assess their clinical significance for the individual patient.
This approach may streamline diagnosis and avoid the excessive use of other neurological testing, including imaging studies of the brain.
How important is it to consider the real world applications when designing a test?
There is no point in offering a clinical test if it won’t advance clinical care. One of the great challenges in medicine today is how to transform mass quantities of genetic sequencing data into clinically relevant information that enhances diagnosis.
Athena’s new epilepsy services represent our commitment to develop test services which align with the real-world clinical approach physicians take to evaluate, diagnose and treat patients across a continuum of care.
What impact do you hope the autoimmune epilepsy test will have?
Early and accurate diagnosis is the most critical piece to the optimal delivery of healthcare services.
A reliable diagnosis and early treatment plan is of obvious benefit to the patient and treating physicians. But it also affords better outcomes, more targeted test utilization and significant potential cost savings for the health care system.
Too many patients experience delayed diagnosis and treatment, and that’s a major health care problem. We believe our new epilepsy tests will help more patients receive earlier diagnosis and treatment for epilepsy.
Where is the test currently available?
All of the new epilepsy tests are available nationally, with the exception of New York, where state approval is expected within the next six weeks.
What are Athena Diagnostics plans for the future?
Athena Diagnostics is the specialty neurology business of Quest Diagnostics. Quest Diagnostics is the world’s leading provider of diagnostic information services, providing testing for about 30% of American adults and about half of the physicians and hospitals in the United States.
Athena focuses on highly sophisticated neurological diagnostics, while Quest focuses on biological tests for neurological disorders. The result is that physicians can access a wide breadth of neurology test services spanning the continuum of care.
This is a unique competency, and we intend to continue to build it in the future because it affords a physician an opportunity to evaluate a patient holistically.
We are also very focused on new services that help physicians care for patients according to medical guidelines and which hasten diagnosis for neurological and rare disorders, particularly those whose outcomes may be favorably influenced with treatment.
Where can readers find more information?
For more information, visit QuestDiagnostics.com or AthenaDiagnostics.com.
About Dr. Joseph Higgins
 Joseph J. Higgins, M.D., F.A.A.N. is medical director of neurology for Athena Diagnostics, a business of Quest Diagnostics.
Joseph J. Higgins, M.D., F.A.A.N. is medical director of neurology for Athena Diagnostics, a business of Quest Diagnostics.
Before joining Athena Diagnostics in February 2012, Dr. Higgins most recently was Professor of Pediatrics and Pediatric Neurology and directed the Weill Cornell Autism Research Program at Weill Cornell Medical College, and was the Principal Investigator of Weill Cornell Autism Research Program.
Prior to that, he served as an Associate Professor in the Department of Biomedical Sciences at SUNY Albany, and as the Laboratory Director of the Clinical Neurogenetics Laboratory at the Wadsworth Center.
He also held a faculty position as a Clinical Associate Professor at Albany Medical College where he evaluated neurogenetic patients at the Center for the Disabled. Before that position, Dr. Higgins served as a Senior Staff Physician with the National Institute of Neurological Disorders and Stroke (NINDS).
Dr. Higgins is U.S. Board Certified in Pediatrics, Psychiatry and Neurology, and Neurology with Special Qualifications in Child Neurology.