May 15 2014
Photodynamic therapy (PDT) is an effective treatment for easily accessible tumors such as oral and skin cancer.
But the procedure, which uses lasers to activate special drugs called photosensitizing agents, isn't adept at fighting cancer deep inside the body. Thankfully, that's changing due to new technology that could bring PDT into areas of the body which were previously inaccessible.
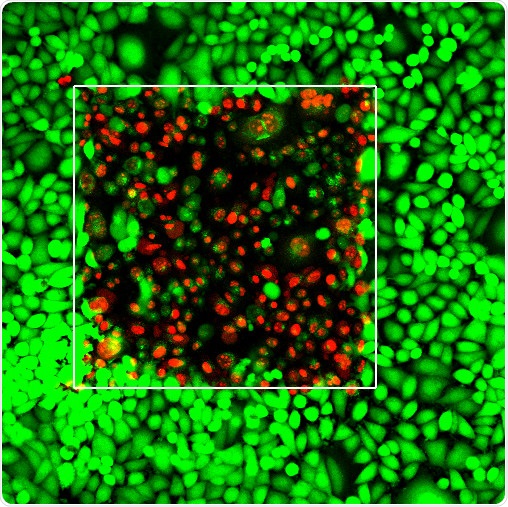
The laser irradiated area (white square) shows live cancer cells (green) as well as dead cancer cells (red) as a result of the irradiation. Credit:University at Buffalo
Described May 11 in the journal Nature Photonics, the approach involves using near-infrared beams of light that, upon penetrating deep into the body, are converted into visible light that activates the drug and destroys the tumor.
"We expect this will vastly expand the applications for an effective cancer phototherapy that's already in use," said co-author Tymish Ohulchanskyy, PhD, University at Buffalo research associate professor and deputy director for photomedicine at the university's Institute for Lasers, Photonics and Biophotonics (ILPB).
Doctors have used PDT to treat cancer for decades. Cancer cells absorb the drug, which is delivered to the tumor via the bloodstream or locally. Visible light is then applied to the site, which causes the drug to react with oxygen and create a burst of free radicals that kill the tumor.
Unfortunately, visible light does not penetrate tissue well. Conversely, near-infrared light penetrates tissue well but doesn't activate the drugs efficiently.
To solve this problem, some researchers are developing drugs that absorb near-infrared light. This method is limited, however, because stable and efficient near-infrared absorbing photosenzitizers are notoriously difficult to synthesize.
The UB-led team took a different approach, which uses the tumor's natural environment to tune the light into the necessary wavelengths.
For example, the near-infrared laser beam interacts with the natural protein collagen, which is found in connective tissues. The interaction changes the near-infrared light to visible light, a process known as second harmonic generation. Likewise, natural proteins and lipids within the cells interact with near-infrared laser light and change it to visible light through another process called four-wave mixing.
Thus, visible light can be generated in tumors deep inside the body, and it can be absorbed by the drug. This activates the drug, which then destroys the tumor.
The procedure has numerous advantages, said the study's leader, Paras Prasad, PhD, SUNY Distinguished Professor in chemistry, physics, electrical engineering, and medicine at UB, and the ILPB's executive director.
"There are no long-term side effects for PDT, it's less invasive than surgery, and we can very precisely target cancer cells," he said. "With our approach, PDT is enriched to provide another tool that doctors can use to alleviate the pain of millions of people suffering from cancer."
UB has applied for a patent to protect the team's discovery, and the university's Office of Science, Technology Transfer and Economic Outreach (UB STOR) is discussing potential license agreements with companies interested in commercializing it.
The research is a collaboration between ILPB, Shenzhen University in China and Korea University in Korea, with which Prasad is affiliated. It was supported in part by a grant from the U.S. Air Force of Scientific Research. Other co-authors are Aliaksandr Kachynski, Artem Pliss, Andrey Kuzmin and Alexander Baev, all PhDs and researchers within ILPB, and Junle Qu, PhD, Shenzhen University.
Source: University at Buffalo