The most common form of diabetes is sometimes referred to as metabolic diabetes, which is the diabetes most people are very familiar with, type 2 diabetes. This form of diabetes is most prevalent in people that are overweight or obese. Historically, it has been confined to adults or older patients but it has been on the rise as the global obesity problem has continued to worsen.
The second most common form is type 1 diabetes, which used to be referred to as juvenile diabetes. Type 1 diabetes is not caused by obesity or other metabolic issues and is an autoimmune disease.
Autoimmune disease refers to when the body's immune system has, for some erroneous reason, recognized a piece of itself as being foreign and started to attack it. In this case, that piece of the self is the pancreas, the organ that makes insulin.
Type 1 diabetes and type 2 diabetes are therefore very different diseases, but they both present with an elevated blood sugar level. In type 2 diabetes, this is because the body has become resistant to insulin, meaning the insulin is ineffective, whereas in type 1 diabetes, the body stops producing insulin altogether because the pancreas is under attack.
The fact that type 1 diabetes is an autoimmune disease means that we can sometimes detect the problems in the immune system before symptoms have manifested, whereas in type 2 diabetes, these immune signs do not occur. We can therefore define biomarkers in the blood that are predictive of type 1 diabetes that are not found in type 2 diabetes.
Do type 1 and type 2 diabetes also differ in terms of treatments?
The therapies that are needed, particularly immediately following the diagnosis stage, can also be very different. There are two elements to this, one regarding where we are right now and another regarding what is coming very shortly in the future.
One issue right now is that when the body does not making any insulin (type 1 diabetes), it starts to become acidotic, which can cause critical illness. This is actually one of the major risk factors for death associated with new-onset diabetes.
You can develop something called diabetes ketoacidosis. This condition can progress rapidly, meaning a person can go from feeling pretty well to suddenly being critically ill and the only way to intervene is to introduce insulin into the equation.
If someone has type 1 diabetes, they need insulin and they need it urgently, or else their disease can progress. Unfortunately, insulin is only given as an injection, so patients have to learn how to give themselves shots. If they're a child, adolescent or even a young adult, this can require hours of training.
Also, because the current testing can take anything from days to weeks, we need to assume that anybody who is at risk of type 1 diabetes has type 1 diabetes, until proven otherwise. That means starting the patient on insulin even though we are not sure what type of diabetes they have.
Where I practice, we are finding that around 25% of pediatric diabetes is actually type 2 diabetes. That means for 25% of cases, we might not have needed to initiate insulin therapy. If we knew they had type 2 diabetes, they could have been seen as an out-patient and maybe not started insulin therapy, thereby avoiding a lot of stress and time spent in hospital.
I'm a pediatrician and it's been obvious to me for about five to ten years that this problem has become worse every year in children, but what we're also seeing is that the rate of type 1 diabetes is actually increasing in the adult population, for reasons that we really don't understand.
We know that the incidence of autoimmune disease in general is on the increase, but we don't know why adults are getting type 1 diabetes. Whereas the condition used to be called juvenile diabetes, this name really is obsolete now because adults are getting type 1 diabetes at a notable rate.
For adults, the situation is then reversed, with people assuming that because the patient is an adult, they must have type 2 diabetes. We may then introduce some exercise, diet modification and maybe an oral medicine, only to find that they don't have type 2 diabetes but type 1 and because they didn't get their insulin, they had a very rough time until their actual diagnosis was eventually figured out. That's why it's so important to distinguish between these two types of diabetes, and the sooner we do so, the better care we can provide to patients.
What's happening now is that clinical trials are being conducted to assess immune modulatory therapies. The aim here is to try to reprogram the mistake the immune system has made and repair it so that type 1 diabetes can at least be less acute. Someday, we may even be able to cure patients with type 1 diabetes if we intervene.
The clinical trials so far indicate that the more quickly we use these new, next-generation therapies, the more effective they are. It appears that waiting weeks might make a significant difference to patients in terms of whether these next-generation therapies are going to be effective or not. That is going to raise the standard and really force us to reconsider how we approach the diagnostic paradigm, so that we can bring these next-generation therapies most effectively to the patients that need them.
Historically, type 1 diabetes was diagnosed almost exclusively in children and type 2 typically affected adults. Why do you think this is changing?
With regard to type 2 diabetes in children, we've been concerned for about a decade that our children, especially in America, are getting obese and that they're going to have medical problems if we let this go on. Unfortunately, that is no longer a fear, but a reality and they actually are developing metabolic diseases.
In California, which is considered a healthier region of the U.S, 25% of the pediatric diabetes population have type 2. There are also regions of the U.S, as well as other regions of the globe, where that number actually hits or exceeds 50%.
There's no doubt that the crossover has occurred and type 2 diabetes is no longer a disease that people only get as adults. The reasons are most likely sedentary lifestyle, poor diet and those types of intuitive problems that we have all been discussing for some time.
In terms of why type 1 is increasing, we have some theories about that and we think this chip might help us understand why, but nobody really knows for sure. The increase is occurring in parallel with increases in some other autoimmune diseases in adults, but that's really a research question.
We know it's happening from an epidemiological standpoint, but the exact reason is still hotly pursued as a research question.
Has this increased the need for better diagnostics to distinguish between type 1 and type 2 diabetes?
Basically, there used to be two more distinct populations. It wasn't that we didn't need to know what type of diabetes someone had, it was just that the epidemiology worked out relatively cleanly, with type 1 usually seen in children and type 2 usually seen in adults. It was fairly safe to assume that, especially if you were dealing with a very young child or an overweight adult.
The way I view it is that there's nothing about obesity that protects you from autoimmune type 1 diabetes, and there's so much obesity now that there's clearly going to be an overlap between people that are obese and those in whom diabetes is caused by autoimmune disease. There's now an increased need for better diagnostics because the epidemiology has really evolved.
Please can you describe the old test used to detect auto-antibodies? How long did this take and why was it is so expensive?
The old test is decades old and it's called radioimmunoassay or RIA for short. RIA is very labor-intensive and expensive, as well as being a biohazard because radioactivity is needed to detect the antibodies.
There are four autoantibodies that can diagnose type 1 diabetes and you actually only need one of those autoantibodies to be positive. Using the RIA test, we can only test for one autoantibody at a time, meaning the patient needs to have four different tests before we can decide if they have type 1 diabetes.
Many people have tried to evolve the platform from RIA to traditional next-generation platforms, which would be similar to an ELISA plate. However, for some reasons that are known and some that are unknown, the testing for these particular autoantibodies is recalcitrant to traditional platforms and trying to move away from RIA really didn't achieve the sensitivity and specificity required for this type of diagnostic. We've therefore been stuck with this very expensive and labor-intensive RIA procedure.
In the U.S, there are grades of laboratories. There are local labs that can handle certain high-throughput, very automated diagnostics and then there are regional labs and national labs. RIA is the type of test that needs sending to a very high-level, national lab because it requires a lot of technical expertise to perform. It takes two to three days of actual hands-on labor to carry out, as well as requiring radioactivity.
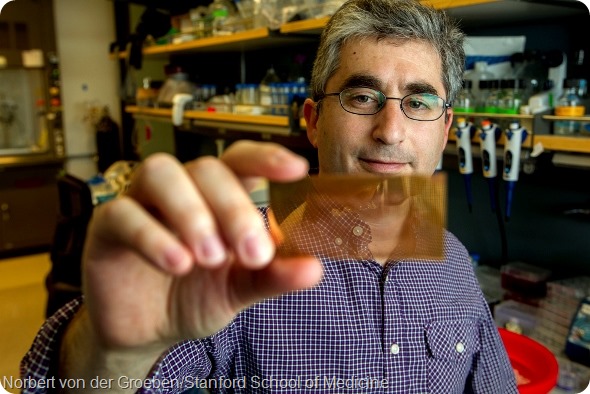
Could you now outline the new microchip-based test you have developed and explain how it differs from the old test?
Right now, the test is performed on top of a glass slide with relatively state-of-the-art surface chemistry. One of the key features is plasmonic resonance, which we use to amplify the signal of the autoantibodies.
In more layman's terms, there's a gold surface that allows plasmonic resonance to occur, which is basically a way to significantly amplify a fluorescent type of signal. On top of that, we have layers of chemistry that preserve the structure of the antigens that are being recognized, allowing them to stay in their more natural state.
One of the reasons the traditional ELISA plates and other next-generation techniques have been unsuccessful is because they fail to preserve this regular structure of these sensitive antigens. We've built that into the surface chemistry of our chip. The plasmonics are also so powerful at amplifying the signal that we can measure the autoantibodies using just one drop of blood. This is quite a contrast to the millilitres of blood required for RIA.
We can also measure all of the autoantibodies simultaneously in a multiplexed fashion using the chip, rather than having to measure each autoantibody individually. Furthermore, the processing time for our chip is about 1 to 1.5 hours, as opposed to several days and the processing skills required are very straightforward, involving fluidics that can be automated.
Another point I would like to make is that because RIA is so costly and technically challenging, type 1 diabetes diagnostics is essentially inaccessible to large reaches of the globe that just don't have the resources or the technical training to carry it out.
Even though this platform is state-of-the-art, it's highly amenable to being mobilized globally, which would provide an exciting opportunity to bring diabetes diagnostics to regions of the globe that can't access the current technology. This would allow people to direct precious resources to where they're needed in a selective way and we hope it will be really helpful.
Why is rapid detection of type 1 diabetes so important?
Currently, there is a need to make sure we find the adults that have type 1 diabetes and don't lose them in the sea of adults with type 2 diabetes. For children, we need to protect the ones that don't necessarily need to start on insulin and cater the therapy to their specific needs.
Knowing somebody's diagnosis from the outset allows you to provide patient-specific care. The care that's provided right now really does not cater for the individual’s needs in the way that it could do if we have this information more rapidly.
In the future, next-generation therapies that are coming online will really demand that we improve the speed at which we obtain this information, in order to provide the most effective care.
Could the nanotech microchip test be used on the population at large to determine a person’s risk of developing type 1 diabetes?
Autoantibodies are very powerful diagnostic tools. They are also one of the most powerful biomarkers of disease that we have available in medicine. Several studies have indicated that each autoantibody present in your body actually increases your risk of developing diabetes in a cumulative manner, even before you know whether you have diabetes.
Current approximations suggest that if one autoantibody is present, you have about a 20% risk of developing diabetes in the future, while if three are present, the risk is above 90%.
That is a really powerful piece of information, both for helping patients understand their own risk, as well as for performing interventional studies and trials on patients that are clearly at risk of developing disease.
I think diagnostic platforms need to be validated rigorously, but predictive platforms even more so. The positive predictive value of tests change depending on what population is tested.
We have not yet conducted the clinical studies that will tell us that, but we hope that this chip will now enable us to screen populations that are not new-onset. The populations that we've studied so far are clearly new-onset diabetes, so our goal is to see how the chip performs in a larger population.
Whether or not diabetes can be prevented from developing in someone who does have an autoantibody is certainly a key research question, but nothing has yet been proven effective.
Probably the most prominent and widely accepted study was an oral insulin therapy trial, which was funded in part by NIH and JDRF. They took patients that were at risk of developing diabetes based on whether they had positive antibodies and used oral insulin to see whether it could reprogram the immune system to recognize insulin as not being foreign.
The study indicated that what's called the “honeymoon period” can be extended in a certain subclasses of patients that have positive autoantibodies. It certainly is not the cure and it wasn't universally effective either, but it showed how knowledge can make a difference, and if we don't have that knowledge, we can't study what therapy might work in these patients.
There are also some indications that other, more potent immunomodulation therapies may actually be preventative, or at least delay the onset of diabetes.
What impact do you think the new nanotech microchip test will have on our understanding of how type 1 diabetes develops?
I think there's a number of different questions we may be able to answer. We really don't understand a lot about the disease, but one example I can give concerns the autoantibodies we have been talking about. These autoantibodies are measured in what's called a binary way, meaning the main thing we focus on is if they are present or absent.
However, people have very different levels of these autoantibodies and that can probably be an indicator of the disease stage or how they would respond to therapy or interventions, for example. So far, we haven't been able to assess these levels of autoantibodies in a high-resolution way as people progress to developing diabetes.
Neither have we been able to properly assess their response to therapy. This platform could enable us to do those things in a cost-effective and rapid way.
We could then measure the level of these autoantibodies in patients that have not yet developed diabetes and follow what happens when disease occurs, as well as looking at what happens when we intervene.
We would be able to see whether the titers of these autoantibodies change and whether that indicates anything about what the body is doing.
I think this highlights how the current technology is interfering with our understanding of the disease. We are working on a very simplistic level where we check the levels of autoantibodies once to establish whether they are present or not and then that’s the end.
There's really so much more to know and learn just simply about the autoantibodies themselves. Other biomarkers can also be discovered using this platform, but I think monitoring titers is an example of something that can be done immediately that was difficult to do on the other platform.
What are your further research plans?
Essentially we will be using the platform to enable studies that were too challenging before such as monitoring autoantibody titers, especially in the setting of immune modulatory interventions, and using the platform to discover new biomarkers. Those are the main areas that we're going to keep working on.
Where can readers find more information?
Our paper was published in Nature Medicine: http://www.nature.com/nm/journal/vaop/ncurrent/full/nm.3619.html
More information can be found on Stanford’s website http://med.stanford.edu/news/all-news/2014/07/researchers-invent-nanotech-microchip-to-diagnose-type-1-diabete.html
About Dr. Brian Feldman
 Brian Feldman, MD, PhD is an assistant professor of pediatric endocrinology and the Bechtel Endowed Faculty Scholar in Pediatric Translational Medicine and a pediatric endocrinologist at Lucile Packard Children’s Hospital Stanford.
Brian Feldman, MD, PhD is an assistant professor of pediatric endocrinology and the Bechtel Endowed Faculty Scholar in Pediatric Translational Medicine and a pediatric endocrinologist at Lucile Packard Children’s Hospital Stanford.
He earned his MD and PhD degrees from Stanford School of Medicine. He received training in Pediatrics at Harvard University at Boston Children’s Hospital and subspecialty training in Pediatric Endocrinology at the University of California, San Francisco.
He joined the faculty at Stanford University in 2009. He has received several awards for his research including the Young Investigator Award from The Society for Pediatric Research, The New Investigator Award from the Endocrine Society and the NIH Director’s New Innovator Award.