The study evaluated cognitive function in patients with colorectal cancer. It characterized the incidence and severity of cognitive impairment in people with colorectal cancer (CRC) compared to healthy controls.
In addition we evaluated patient reported outcomes including perceived cognitive function, fatigue and quality of life, and evaluated underlying mechanisms including cytokines, blood clotting factors, sex hormones and apolipoprotein genotyping.
Assessments were completed soon after diagnosis but prior to receiving any chemotherapy or radiotherapy, and at 6, 12 and 24 months.
A total of 289 patients with localized CRC, 73 with metastatic CRC and 72 healthy controls completed baseline assessments. There was more cognitive impairment in people with localized CRC than healthy controls at every time point, but no significant effect of chemotherapy on cognitive impairment.

The study found colorectal cancer patients are up to three times more likely to suffer cognitive impairment compared to non-cancer sufferers. What types of cognitive impairment were recorded?
Attention/working memory, verbal learning/memory, and complex processing speed were the cognitive domains most affected.
Were there any differences in the cognitive impairment found in women and men?
This is the first study to be able to look at cognitive gender differences in cancer patients. We found that in colorectal cancer patients women have higher rates of cognitive impairment but men are more likely to have deterioration in cognitive function with time.
Did you find that chemotherapy impacted cognitive impairment?
Interestingly, no significant differences were seen in objective cognitive function at any time point in those who received adjuvant chemotherapy, compared to those with lower stage disease who did not require chemotherapy.
Were you surprised by these findings or are they in line with previous studies?
Baseline cognitive impairment (prior to chemotherapy) has been seen in a number of studies in women with breast cancer. Although there are inherent difficulties with comparing rates of impairment between studies, if anything the impairment rate at baseline (42% compared to 15% in healthy controls) seemed higher than the rates of impairment seen in the majority of breast cancer studies.
The main surprise was the lack of significant difference on objective cognitive impairment between those who received chemotherapy and those who did not. We analyzed the cognitive impairment in a number of ways, looking at individual tests, cognitive domains and global impairment but failed to find major differences between the groups.
Our hypothesis was that elevated cytokines would be associated with cognitive impairment, but we found no consistent association. Interestingly, an interim analysis did find an association but with the full sample size this was no longer significant.
How much is currently known about the underlying mechanisms?
The cause of cognitive impairment in cancer patients is unknown. A number of animal models have found that a number of different chemotherapy agents cause cognitive impairment, however in our large clinical study we did not find a difference.
Other smaller studies in women with breast cancer have suggested an association with cytokines, but we found no association.
Possible explanations may be that some other studies have looked at other cytokine receptors, whereas we evaluated the cytokines using a multiplex platform. Similarly we found that apolipoprotein E genotyping was not associated with cognitive impairment, whereas smaller studies have suggested an association.
Where should future research focus in order to increase our understanding of the underlying mechanisms?
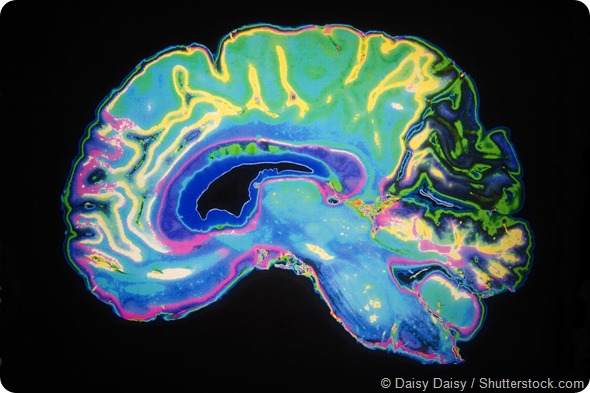
Ongoing studies in animal models will be important but ultimately we need clinical studies. Functional imaging studies are providing important information about changes seen in patients who receive chemotherapy.
Ideally to progress the field we need to combine data from multiple international researchers to be able to obtain large sample sizes. The International Cognition and Cancer Task Force (ICCTF) has been working to achieve this.
How can health professionals help patients prepare for and cope with memory loss?
Patients need to be advised that cognitive impairment is a possible side effect of cancer and cancer treatment. Health professionals can also assist by using techniques to help patients remember information discussed at consultations. As there is an association between cognitive symptoms and fatigue, anxiety and depression it is important to also assess for these symptoms, and if present to treat them.
At what point should patients be referred to a neuropsychologist?
In an ideal world we would have formal neuropsychological assessment on everyone, however most hospitals and cancer centers do not have these facilities. If patients notice ongoing symptoms after completion of treatment, and fatigue, anxiety and depression have been assessed, and if present treated, then it would be helpful to obtain a neuropsychological assessment to determine if cognitive impairment is present and where the deficits are.
What should a patient do if they are worried about cognitive impairment and where can readers find more information?
For many patients any cognitive impairment that is present is subtle and will often improve with time away from treatment. At present there is no evidence on how best to treat this.
A number of studies are underway to try and provide better information on how to prevent cognitive impairment from occurring and/or to treat it after it has occurred – this includes assessing cognitive rehabilitation programs.
Compensatory strategies may help patients to cope with cognitive symptoms. This includes things like making notes and use of smart phones/diaries for reminders, minimizing distractions, trying to work on one task at a time.
Information can be found at the ICCTF website (icctf.org) as well as on a number of cancer organization websites.
About Associate Professor Janette Vardy
A. Prof Janette Vardy is a medical oncologist in Sydney, Australia. She leads the Sydney Survivorship Centre at Concord Cancer Centre, and together with Dr Haryana Dhillon, co-leads the Survivorship Research Group at the University of Sydney. Their major research focus is on cognitive function in cancer patients and physical activity in cancer survivors.