Adherence applies to multiple levels of healthcare. Before a drug goes on the market it has to undergo testing in clinical trials: participants take the study drug and report how well the drug works, along with any side effects.
The problem is that often study participants don't take the drug correctly according to the protocol, and sometimes they don’t take the drug at all. This can jeopardize trial results since at the end, investigators don’t know when or if study participants took the drug.
In population health, people go to the doctor to get a prescription, but when it comes to taking the prescription, we're not always that good at seeing it through. People often don't take their medication for different reasons, whether it be laziness, forgetfulness, side effects, or starting to get better and believe the medication is no longer needed.
What problems does non-adherence cause in the patient population?
Across all patient populations, it is clear that medications are prescribed to relieve symptoms and improve patients’ health. But in order to benefit fully from the medication, patients need to take it exactly according to the doctor’s instructions.
However, patients may take their medication at the wrong time, forget to take it, or choose not to take it. When patients don't take their medication, the disease or the condition can be prolonged or it can lead to complications making the patient more ill; or, if the condition is serious, lead to costly hospitalizations or emergency room visits. But if patients take their medication the way they're supposed to, many of these high-cost complications can be eliminated.
For those patients who are at high risk of poor adherence and for whom poor adherence can have drastic consequences, it is particularly important they receive accurate monitoring and support. Preemptive interventions based on real-time data can make a huge impact on the health of the patients and on the healthcare system.
Close to $300 billion are wasted due to non-adherence. For certain conditions, a single dose of medication can cost hundreds of dollars, and a year’s worth of medication can add up to hundreds of thousands of dollars. For many patients, across all therapeutic areas, every dose matters.
What problems does this cause for the clinical trial industry?
In clinical trials it’s a bit more complex because the implications are far greater and they really affect everybody. Everyone who will ever take a medication in the future is affected by what happens within a clinical trial.
If the study drug is not taken during a clinical trial, essentially what's happening is that it’s not being properly tested. If patients don’t take the study drug, you won’t know whether the drug works or what levels of the drug are safe. These are the two biggest problems. There is a high failure rate in clinical trials and one of the reasons is non-adherence. Hundreds of millions of dollars are spent on each trial; some drugs take over a billion dollars to develop. It is critical for the industry to ensure drugs are properly tested.
Another problem is the trial being delayed because of non-adherence. Poor adherence by study participants may require investigators to increase enrollment, leading to higher costs and significant delays. Each day the drug is delayed from being released onto the market translates into huge losses for the industry by reducing the drug’s patent life.
Longer and more costly trials can delay life-saving treatment reaching patients. And poorly tested drugs can result in unexpected side effects in the general population that may only be discovered once the drug is approved and taken by tens of thousands of patients.
Can you give me a brief description of AiCure, how it works and what it does to increase medication adherence?
We built a platform using advanced, artificial-intelligence techniques that help those running trials, and physicians working in general population health, to know when individuals are taking their medication. That's one side of the coin.
AiCure's artificial intelligence visually confirms medication ingestion www.aicure.com
AiCure's artificial intelligence visually confirms medication ingestion www.aicure.com from AiCure on Vimeo.
The other side of the coin is that our platform helps participants in trials and patients remember to take their medication, and encourages them to take their medication. It's a platform that helps increase adherence, and monitors adherence both for clinical trials and for population health.
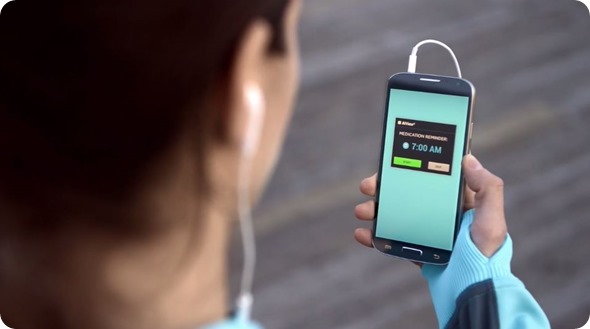
More specifically, we've developed an app that uses computer-vision techniques. The app works on low-cost, standard consumer mobile phones and uses the camera to verify, automatically and in real time whether the patient is taking the medication.
More specifically: the patient (or participant in a clinical trial) takes their phone or tablet, either Android or iOS. They lift it up so that it's facing them, and showing the image that's being captured with the camera. The patient then takes the medication, holds it up to the camera, and ingests the medication.

The mobile device automatically, using artificial intelligence and without any human intervention, verifies that the patient took the medication.
What features are used to ensure that a patient or clinical trial participant is taking their medication properly?
What the app is actually doing in the background is the following: it's recognizing the person using the app, using facial recognition; it's recognizing the pill to make sure that it's the right pill that the patient is taking; and it's verifying that he or she is taking the pill.

The app is designed for any patient in any therapeutic area. Since it is software-based it is fully flexible and customizable according to the patient population, the disease, and other individual characteristics.
It also adapts to patient behavior over time. Since medication adherence is a complex problem, we wanted to create a solution that could address the many determinants of non-adherence and not have a simple one size fits all approach. These tend not to have much impact on either adherence or health outcomes.
When it’s time for you to take your medication, you'll get an alert to take your next dose. If you're taking multiple medications, it will tell you which ones you have to take.
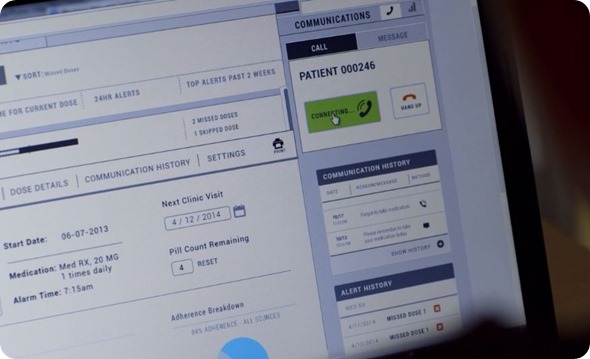
It's doing all of this automatically without any human intervention on the phone or device itself. Then it's automatically sending data to a dashboard, to multiple dashboards actually which depend on the use case.
In clinical trials, research staff will have access to a dashboard listing all of their study participants and indicating adherence in real time. In population health it works the same way. A hospital or health system, for example, can access the dashboard and view all patient adherence data.
In both clinical trials and population health, the dashboard is used for monitoring and intervention. Research staff or healthcare workers will be notified in real time when patients are non-adherent, making intervention more efficient and less resource-intensive since not all patients need to be monitored all the time. Only those requiring help or at risk of non-adherence will receive an intervention. In addition to adherence data, side effects or health outcomes can be tracked and correlated with adherence.
We’ve found that using the app alone increases patient adherence because it not only helps users remember to take their medication but it seems to have an effect where it increases their responsibility to themselves to take the medication.
Is AiCure for pills only? Are there other treatment modalities that can be recorded?
Yes, we have several modules for inhalers and other kinds of medications and we're increasing our technical footprint to work with other types of medications. In essence we will cover all medications that are visible.
When you swallow a pill, take a sub-lingual medication or use an inhaler it's visible. We’re also working with injectable pens and a bunch of other things.
How possible do you think it is for a patient or clinical participant to cheat the app? How have people tried to cheat the app?
The technology has several levels of security embedded in the device when it's deployed that are meant to detect any kind of cheating. Face recognition is one example of that. One of the problems in clinical trials, is that sometimes people enroll in multiple clinical trials because they're getting paid.
The face-recognition technology helps us identify whether the person participating in a trial is already involved in another conflicting trial. It also verifies that the person who is supposed to be completing the trial is the one taking the tested drug. When you register you want to make sure that the right person is taking the study drug.
There are many other things that people can do to try to cheat when they take medication. The app detects a whole list of different activities to ensure that the patient is not cheating. In general, the level and type of cheating people might try, depends on the patient population of the condition being treated.
For example, somebody taking an anticoagulant after a stroke is much less likely to cheat than a patient undergoing addiction treatment. These are two extremes. In one case, the motivation to cheat is very low. In the second case motivation might be quite high. Depending on the use case and population target we have different settings, thresholds and screening mechanisms so that it'll be stricter with those groups where cheating is more likely.
It’s similar to the human equivalent, for example with directly observed therapy - where a nurse watched you take your medication - if you try to cheat once and the nurse catches you, the nurse will be much more vigilant when you're trying to cheat the next time.
The platform has built-in intelligence to deal with these behavioral patterns. We've done a lot of work investigating the psychology of cheating, adherence and to understand how people's use of the app might change their behavior, how they would behave again within certain contexts.
What happens if a patient or participant is thought to be cheating on their prescription or is forgetting to take medication?
If a patient or trial participant is not taking their medication correctly for any reason, whether they simply forget or whether the nonadherence is intentional, the platform detects the patterns and sets up automated alerts within the dashboards so that investigators or doctors will see all data relating to individual cheating attempts or misses and also the patterns.
Understanding patient behavior over time, continuous real-time data, can give you a very rich understanding of how the patient is progressing. Big data and predictive analytics are a fundamental component of the platform.

To give you an example, the response to a patient who’s been taking their medication and using the app properly 99 times, but gets an alert of cheating on the 100th time, would be different from responding to alerts for a patient with a pattern of cheating attempts every third time they take the medication.
Typically since the dashboard is reporting adherence and usage of the technology on the part of the patient, the physician or site running the trial has the ability to contact the patient directly and say, "Looks like you're having a problem with the app. What's going on?" or "You haven't taken your medication today, is everything okay?"
A lot of thought has gone into how that works, including the state of mind of the patients, as we don’t want to unnecessarily intervene. Depending on the type of alert, we have anonymized systems in place to do a human review of the interactions with the app to double check patterns that may need to be reviewed.
What does the future hold for AiCure?
We've, of course, done a lot of deployments and studies. We've gotten feedback both from patients and clinical trial participants, and the feedback is overwhelmingly positive.
We’ve paid a lot of attention to the design of the app and made it user friendly, to make sure that it's multi-cultural, that it works at any literacy level, and can be deployed anywhere in the world, both for clinical trials and for population health.
It's completely scalable because in both cases the apps can be downloaded from the App Store or Google Play which means the distribution part of it is scalable already at a global level. It is also robust in connectivity, if a patient is using the app without WIFI or a network connection, they can still use it and the data will be uploaded when they're connected.
The scalability means that, in terms of future clinical trials, we'll be able to deploy very large-scale clinical trials and segment the population, leading to more personalized medicine. Then, we'll be able to know and track side effects in narrow segments of the population. That's super exciting, the idea that we can scale that way.
We'll be able to speed-up clinical trials and become more accurate, making them more effective and less expensive. With our technology you're able to detect early-on in the trial if one of the participants is not taking the medication and you can quickly replace them.
In the past, the challenge has always been the technology. Now, almost everyone in the world has a smartphone, 6 billion phones are projected to be in people's hands by 2020. Everyone can potentially participate in a clinical trial; but more importantly, any patient no matter where they are can benefit from this sort of technology. We hope to help patients worldwide, improve adherence and change their behavior.
Before smartphones, it was very hard to do this. You had to get the device in people's hands, you had to change manufacturing processes. Right now, because the computational ability that we have on the phone itself, being able to run face recognition, algorithms that rely heavily on machine learning and big data to automatically recognize pills, this is pretty incredible. We couldn't do this ten years ago, the devices didn't exist.
The knowledge and data obtained will open up the possibilities of personalized medicine in new and exciting ways. It will also allow for insights into population health that have never been seen before as we connect patients to better treatment and improved health. We want to revolutionize healthcare, and our current product embodies the beginnings of an Artificial Intelligence medical assistant that adapts and leads to personalized medicine in novel ways.
Where can readers find more information?
Please visit: AiCure.com
About Dr Alejandro (Alex) Jaimes
Alejandro (Alex) Jaimes is an expert in Artificial Intelligence, with a focus on Machine Learning and Computer Vision. Dr. Jaimes has over 100 publications and patents, and is well known internationally for his work on Human-Centered Computing.
He has over 15 years of international experience in research and product impact (Yahoo, KAIST, Telefonica, IDIAP-EPFL, Fuji Xerox, IBM, Siemens, and AT&T Bell Labs), building Data Science and Engineering teams across continents and deploying products at scale.
He has worked in the USA, Japan, Chile, Switzerland, Spain, and South Korea. He holds a Ph.D. from Columbia University.